Procedure Coding: Location, Location, Location
Coding Paths Diverge
In addition to the patient’s diagnosis, the other pieces of information associated with every healthcare encounter are the procedure codes, the dates the procedures were performed, the location in which they were performed, and the physician or other provider who performed them.
The term procedure coding encompasses a wide variety of services to patients:
![]() Surgery: Operative treatment of disease or injury
Surgery: Operative treatment of disease or injury
![]() Anesthesia: The process of blocking pain or other perceptions
Anesthesia: The process of blocking pain or other perceptions
![]() Radiology: The use of imaging modalities for diagnosis, interventional techniques, or radiation therapy for treatment
Radiology: The use of imaging modalities for diagnosis, interventional techniques, or radiation therapy for treatment
![]() Laboratory: Testing performed on biological specimens to get information about the health of a patient
Laboratory: Testing performed on biological specimens to get information about the health of a patient
![]() Pathology: Diagnosis of disease based on the gross and microscopic examination of cells and tissues
Pathology: Diagnosis of disease based on the gross and microscopic examination of cells and tissues
![]() Diagnostic testing: Nonlab, nonradiologic testing to arrive at a diagnosis
Diagnostic testing: Nonlab, nonradiologic testing to arrive at a diagnosis
![]() Evaluation and management: “Visits” to evaluate patients and manage their care
Evaluation and management: “Visits” to evaluate patients and manage their care
![]() Psychiatric: Treatment of mental or emotional disorders
Psychiatric: Treatment of mental or emotional disorders
![]() Osteopathic: Branch of medicine that uses manipulative techniques to supplement treatment of disease
Osteopathic: Branch of medicine that uses manipulative techniques to supplement treatment of disease
![]() Chiropractic: Focuses on spinal function to improve health
Chiropractic: Focuses on spinal function to improve health
![]() Rehabilitation: Physical, occupational, speech, and other therapies to improve functioning
Rehabilitation: Physical, occupational, speech, and other therapies to improve functioning
![]() Alternative: Diagnostic or treatment methods with theoretical bases that differ from conventional medicine, such as acupuncture
Alternative: Diagnostic or treatment methods with theoretical bases that differ from conventional medicine, such as acupuncture
![]() Preventive: Actions, such as vaccinations, to prevent disease or injury
Preventive: Actions, such as vaccinations, to prevent disease or injury
All types of providers, whether facilities or individual practitioners, use ICD-10-CM diagnosis codes. This is not true for procedure or supply codes. The type of billing code used depends on several factors:
![]() Location, or site of service where the procedure was performed
Location, or site of service where the procedure was performed
![]() Type of charge being coded:
Type of charge being coded:
![]() Professional
Professional
![]() Facility
Facility
![]() Dental
Dental
![]() Durable medical equipment, prosthetics, or supplies
Durable medical equipment, prosthetics, or supplies
![]() Drugs and biologics
Drugs and biologics
In this chapter, we will focus on procedure coding for professional services and facility services.
Hospital Procedures Versus Doctor’s Procedures
As a case study, let’s assume that you have always been in good health, but that over the weekend you started having pain in your stomach region. It started near your navel and then became more and more severe as it moved toward the lower right side of your abdomen. You decided to go to the emergency room. After the exam and some lab work, the doctor decided that you had appendicitis. A surgeon was contacted, and you were taken to the operating room for an appendectomy, or removal of your appendix.
From the time you entered the emergency room to the time you were discharged home after recuperation from your surgery, the hospital maintained a medical record documenting every occurrence during your stay. In addition to documentation by the emergency room physician and the surgeon, your medical record also includes notes by the nursing staff; orders from physicians; reports of diagnostic testing results, such as lab work; administrative paperwork, such as consent forms; visits by allied health personnel, such as the dietitian; your vital signs; and details such as whether you went to the bathroom.
The surgeon who removed your appendix will also start a medical record for you at his office, even though you have not yet been there. At this point, it will probably contain a copy of the operative report dictated by the surgeon for the hospital record and a copy of the hospital “face sheet” of demographics with your name, address, and insurance information. When you visit the surgeon for a follow-up visit after your surgery, he will add a progress note to his office chart.
After you are discharged from the hospital, your medical record will be processed by the facility’s health information department. If the facility is still using paper records, the chart will be assembled into a standard order, checked for missing documentation and signatures, placed in a folder, and the diagnoses and procedures coded. In an increasing number of hospitals, all of the documentation is maintained electronically, in which case many signature and report deficiencies are automatically identified and the provider notified.
As a patient, you are issued a unique number under which all of your health information is maintained. These numbers are specific to a facility or chain of facilities; they are not used across organizational boundaries, with a few exceptions. Known as a patient number, medical record number, or patient identifier, this unique number follows you throughout your care. Patients who are admitted to the hospital as inpatients generally receive a wristband with their name and medical record number. This is used to prevent identity errors and resulting incorrect medication administration, wrong surgery, or lab specimen errors.
Medical coding analysts will look at your record in order to assign ICD-10-CM diagnosis codes to your diagnosis “acute appendicitis,” and they will also assign ICD-10-PCS procedure codes to your procedure “appendectomy.” They may also check the results of the surgical pathology examination of your appendix to determine whether you actually had appendicitis. The diagnosis and procedure codes will be routed to the hospital business office, where a bill will be generated for the facility charges incurred during your stay. If you have insurance, a claim with the diagnosis and procedure codes will be sent to that payer for reimbursement.
Meanwhile, the surgeon is also interested in getting paid. The surgeon’s claim form to your insurance company will usually contain the same ICD-10-CM diagnosis codes used by the hospital, but the procedure code will be different. The surgeon will use Current Procedural Terminology, also known as CPT.
Why the Difference? How Did It Come About?
HOSPITAL PROCEDURE CODING
Coding started as a way to categorize deaths. It evolved into a method of indexing hospital diagnoses and procedures in order to assess the healthcare status and needs of the living. The first advocate of hospital statistics was Florence Nightingale, the famous nurse (Figure 3-1).
While serving in a battlefront hospital during the Crimean War of the 1850s, Nightingale observed that far more soldiers died of disease than of war injuries. Her relentless efforts to improve sanitation helped reduce the mortality rate in her hospital from 33% to 2% in 1 year, 1855 (Gill & Gill, 2005). When she returned to England after the war, she submitted a statistical report to the British government, hoping to convince them that improvement of sanitary conditions in local hospitals would also reduce deaths. The government refused to allow her to publish her data. She persisted, using army data already available, informing the public of her cause. When she began her campaign, life expectancy in England was 39 years. When she died 50 years later in 1910, it had risen to 55, at least, in part, due to her efforts (Small, 1998).
Before 1960, hospitals used various systems to index procedures. With the manual methods in use at that time, “indexing” literally meant using index cards. A card was set up for each procedure code or category, and the medical record numbers of patients who underwent that procedure were written on the card, along with the date of the procedure. At the same time, statistical reports were prepared showing how many of various procedures were performed monthly or annually. If researchers needed information on cases from a particular procedure category, the medical records could be pulled based on the information in the indexes.
The first revision of the International Classification of Diseases (ICD) that contained procedure codes was a version of ICDA-7 issued by the U.S. Public Health Service in 1959. It contained procedure codes with up to three digits. ICDA-8, also with three-digit codes, was used from 1970 to 1978, and ICD-9-CM has been in effect since 1979 and will be until 2015. The latter classification was expanded to four-digit codes for procedures. Starting on October 1, 2015, ICD-10-PCS (Procedure Coding System) goes into effect, with more than 71,000 procedure codes, each containing seven characters.
Concurrent with the development of consistent procedure coding systems was the initiation of the Uniform Hospital Discharge Data Set (UHDDS). Although vital statistics data, such as births, deaths, and marriages, had uniform definitions in the United States, there was no agreement before 1973 on what data should be collected and reported by hospitals. The NCHS collected hospital data, but the emphasis was on the institutions’ overall activities, not the problems of their patients. The statistics described how busy they were, but not what they were accomplishing in the way of patient care (White, n.d.).
An amendment to the Public Health Act in 1974 made the National Committee on Vital and Health Statistics a statutory body and required that there be an annual report to Congress on the health of the American people. Health United States 1975 (Figure 3-2) was a hit with the press (U.S. Department of Health, Education, and Welfare, 1975).
It reported in one place, for the first time, 603 pages of health-related data, such as the average physician fee for an initial office visit ($12.17 for a pediatrician and $17.62 for a surgeon) and the average net income of physicians ($43,570 for a pediatrician and $62,320 for a surgeon).
Hospital discharge data by diagnostic category was skimpy, and there was no information about hospital procedures except for the number of hospitals reporting various types of services, such as burn units, home care, renal dialysis, and blood banks.
FIGURE 3-2 Health United States 1975.
Reproduced from National Center for Health Statistics. Health, United States, 1975. DHEW Publication No. (HRA) 76-1232. Rockville, Maryland. Courtesy of CDC.
Currently, the UHDDS Procedure Code Guidelines, developed in 1973 and revised in 1985, govern the types of procedure code data collected on hospital inpatients. Additional rules developed by Medicare with the advent of its Prospective Payment System (PPS) have come into play because of the link between procedure coding and reimbursement.
PHYSICIAN PROCEDURE CODING
Prior to 1981, a number of different systems were used to code physician procedures. There was no requirement that a code number be submitted with a claim for payment, so many physicians merely submitted a verbal description of what they had done. This required the insurance companies to figure out what some of the arcane descriptions meant before they could decide how much to pay.
When Medicare was enacted in 1965, physicians looked for a better system to report their services. What better group to design a physician coding system than their own professional organization, the American Medical Association (AMA). The first edition of Current Procedural Terminology (CPT) was published by the AMA in 1966. Primarily containing surgical procedure codes, with smaller sections on medicine, laboratory, and radiology, it consisted of four-digit code numbers.
Expansion of CPT led to the following:
![]() Adoption of five-digit codes in CPT-2 (1970)
Adoption of five-digit codes in CPT-2 (1970)
![]() Addition of modifiers for further specificity in reporting in CPT-3 (1973)
Addition of modifiers for further specificity in reporting in CPT-3 (1973)
![]() Inclusion of additional codes for new technology in CPT-4 (1977)
Inclusion of additional codes for new technology in CPT-4 (1977)
In 1992, the Evaluation and Management (E&M) codes were added to describe cognitive efforts involved with nonsurgical services. CPT is updated annually to reflect changes in medical and surgical services.
In 1983, the federal government entered into an agreement with the AMA that CPT would be the mechanism for reporting physician services under Medicare. As is usually the case, other payers followed Medicare procedures and by 1990 CPT had become the single uniform system for reporting of physician services. Today, it is estimated that over 95% of services provided by physicians are reported using the CPT coding system (Harris, 1997).
Whereas ICD-10-PCS is a system in the public domain, CPT remains a proprietary system owned and operated by the AMA. It is not possible to obtain a copy of CPT without purchase.
What About HCPCS?
This system (pronounced “hic-pics”) is the Healthcare Common Procedure Coding System. CPT is considered a part of HCPCS, known as Level I. There are also more than 6,000 alphanumeric Level II codes, which are used to identify healthcare equipment and supplies and drugs (CMS, 2014b). Level II code descriptors identify similar items or services, rather than specific brand names. For example, HCPCS code J3410 has the description of “Injection, hydroxyzine HCL up to 25 mg.” This code does not vary, even if the drug administered is a brand name formulation rather than a generic. The same code is used regardless of manufacturer or supplier. If you visit your doctor and he administers a medication to you during the visit, his claim form to the payer will include a CPT code for his service plus a HCPCS Level II J code for the medication. Retail pharmacies use yet another coding system, the National Drug Codes (NDC). Under consideration is the elimination of the HCPCS J codes and the requirement that all providers and suppliers use the NDC codes. The NDC codes are 11 digits long, which is problematic for the billing systems in many doctors’ offices.
Dental codes, Current Dental Terminology (CDT), are also part of HCPCS Level II. CDT is maintained by the American Dental Association and is used only for dental billing.
“Miscellaneous” and “temporary” HCPCS Level II codes change frequently and are used for new items or services that haven’t yet made it to the permanent section of codes. Miscellaneous codes can be used to bill for items for which no other codes exist.
The fact that CPT is part of HCPCS, and the existence of the 1983 agreement that the AMA would have the “sole responsibility and authority to revise, update, or modify” CPT and to “continue to print, publish, sell, and otherwise disseminate” (U.S. Department of Health and Human Services, 1998) CPT even though it is being used as part of a required code set for federal health program billing purposes has caused accusations that the government “granted the AMA what has been characterized as a ‘statutory monopoly’… a financial windfall for the AMA in the form of CPT-related book and CD sales with revenue of more than $71 million a year” (Lott, 2001).
The Health Insurance Portability and Accountability Act (HIPAA) of 1996 requires, under its Administrative Simplification section, that the Department of Health and Human Services define national standards for the electronic transaction of healthcare information, including provider and facility claims. As of October 16, 2003, standard code sets had to be implemented by all parties who transmit information electronically. ICD-9-CM was the standard code set for diagnoses, whereas ICD-9-CM procedure codes were the rule for inpatient hospital procedures, CDT for dental services, and HCPCS (including the AMA-controlled CPT) was for the following services:
![]() Physician services
Physician services
![]() Physical and occupational therapy services
Physical and occupational therapy services
![]() Radiological procedures
Radiological procedures
![]() Clinical laboratory tests
Clinical laboratory tests
![]() Other medical diagnostic procedures
Other medical diagnostic procedures
![]() Hearing and vision services
Hearing and vision services
![]() Transportation services, including ambulance
Transportation services, including ambulance
The designation of CPT as a standard code set under HIPAA further reinforced its position as a major procedure coding authority. In 2009, the Final Rule was published, changing the diagnosis coding system to ICD-10-CM and the hospital inpatient procedure coding system to ICD-10-PCS (“HIPAA Administrative Simplification,” 2009). No change was made to CPT as the standard code set for physician and ancillary services billing. The original effective date of this change was October 1, 2013, but the secretary of Health and Human Services authorized a 1-year delay to 2014. On April 1, 2014, another delay was enacted as part of a patch to the sustainable growth rate (SGR) Medicare payment formula, postponing the implementation of ICD-10-CM and ICD-10-PCS until October 1, 2015.
Where It’s At
The location where the service or product is provided determines which procedure code set is used. As is the case with many other facets of healthcare billing, the methods of identifying the location differ between professional claims and facility claims. Professional billing uses place of service codes defined by the CMS (CMS, 2012). Facility billing uses the concept of “bill type,” a four-digit alphanumeric code where the second digit represents the type of facility, the third digit represents the classification (clinics only), and the fourth digit equals the frequency of the bill. The first digit is always a leading zero (CMS, 2014a). The following table shows the correlation between bill type and place of service. The character X is used as a placeholder for the fourth digit, indicating bill frequency.
Bill Type |
Place of Service (Location) | |
011X |
Hospital inpatient Part A or |
21 (inpatient hospital) or |
012X |
||
013X |
Hospital outpatient |
22 (outpatient hospital) or |
Skilled nursing |
31 (skilled nursing facility) | |
033X |
Home health |
12 (patient home) |
071X |
Rural health clinic |
72 (rural health clinic) |
072X |
Freestanding dialysis center |
65 (end-stage renal disease facility) |
075X |
Comprehensive outpatient rehab |
62 (comprehensive outpatient rehab facility) |
076X |
Community mental health center |
53 (community mental health center) |
083X |
Hospital outpatient ASC (ambulatory surgical center) |
24 (ambulatory surgical center) |
Source: Data from CMS Publication 100-4 Medicare Claims Processing Manual, Chapter 25, 2013. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c25.pdf.
A number of additional professional services place of service or location codes are available, including the following:
03 |
School |
04 |
Homeless shelter |
09 |
Prison or correctional facility |
11 |
Doctor’s office |
13 |
Assisted living facility |
14 |
Group home |
17 |
Walk-in retail health clinic |
25 |
Birthing center |
26 |
Military treatment facility |
32 |
Nursing facility |
33 |
Custodial care facility |
34 |
Hospice |
55 |
Residential substance abuse treatment facility |
56 |
Psychiatric residential treatment center |
71 |
Public health clinic |
The location or place of service is important in coding because many payers have different reimbursement schedules, copay amounts, or coverage limitations depending on where the service is provided.
The Evaluation and Management (E&M) codes in CPT are defined based on location:
![]() Hospital inpatient
Hospital inpatient
![]() Office or other outpatient
Office or other outpatient
![]() Hospital observation
Hospital observation
![]() Emergency department
Emergency department
![]() Nursing facility (skilled, intermediate, long-term care, psychiatric residential treatment center)
Nursing facility (skilled, intermediate, long-term care, psychiatric residential treatment center)
![]() Boarding home, custodial care, assisted living
Boarding home, custodial care, assisted living
![]() Home (private residence)
Home (private residence)
ICD-10-PCS Procedure Coding Guidelines
HOSPITAL INPATIENTS ONLY
Item 12 of the UHDDS guidelines states that procedure codes and dates of all significant procedures are to be reported (Federal Register, 1985). The identity (number) of the person performing the procedure must also be reported.
What is a “significant procedure”? A significant procedure can be one or more of the following:
![]() Surgical in nature:
Surgical in nature:
![]() Incision
Incision
![]() Excision
Excision
![]() Amputation
Amputation
![]() Introduction
Introduction
![]() Endoscopy
Endoscopy
![]() Repair
Repair
![]() Destruction
Destruction
![]() Suture
Suture
![]() Manipulation
Manipulation
![]() Carries a procedural risk:
Carries a procedural risk:
![]() Professionally recognized risk that a procedure may potentially cause body impairment, injury, disease, or death
Professionally recognized risk that a procedure may potentially cause body impairment, injury, disease, or death
![]() Trauma risk: Procedures that are invasive, able to produce tissue damage, or introduce toxic or noxious substances
Trauma risk: Procedures that are invasive, able to produce tissue damage, or introduce toxic or noxious substances
![]() Physiologic risk: Procedures that use any drug or physical substance that can affect the body
Physiologic risk: Procedures that use any drug or physical substance that can affect the body
![]() Any procedure using pre- or postoperative medications
Any procedure using pre- or postoperative medications
![]() Procedures that use long-life radioisotopes
Procedures that use long-life radioisotopes
![]() Carries an anesthetic risk:
Carries an anesthetic risk:
![]() Any procedure using general anesthesia
Any procedure using general anesthesia
![]() Any local, regional, or other type of anesthesia causing functional impairment that requires care in usage to protect the patient from harm
Any local, regional, or other type of anesthesia causing functional impairment that requires care in usage to protect the patient from harm
![]() Requires specialized training:
Requires specialized training:
![]() Specialized professionals, qualified technicians, or clinical teams specifically trained for the performance of the procedure
Specialized professionals, qualified technicians, or clinical teams specifically trained for the performance of the procedure
SELECTION OF PRINCIPAL PROCEDURE
The principal procedure is defined in the UHDDS as “one that was performed for definitive treatment rather than one performed for diagnostic or exploratory purposes, or was necessary to take care of a complication. If there appear to be two procedures that are principal, then the one most related to the principal diagnosis should be selected as the principal procedure.”
Selection of the principal procedure is related to inpatient reimbursement. Because there is the potential of manipulating coding in order to receive a higher reimbursement rate, additional coding guidelines for the selection of principal procedure and sequencing of other procedures were developed as part of ICD-10-PCS.
Principal Procedure | |
Procedure performed for definitive treatment of both principal diagnosis and secondary diagnosis |
Procedure performed for definitive treatment most related to principal diagnosis |
Procedure performed for definitive treatment and diagnostic procedures performed for both principal diagnosis and secondary diagnosis |
Procedure performed for definitive treatment most related to principal diagnosis |
Diagnostic procedure performed for the principal diagnosis and a procedure performed for definitive treatment of a secondary diagnosis |
Diagnostic procedure performed for the principal diagnosis |
No procedures performed that are related to principal diagnosis; procedures performed for definitive treatment and diagnostic procedures performed for secondary diagnoses |
Procedure performed for definitive treatment of secondary diagnosis since there are no procedures (definitive or nondefinitive treatment) related to principal diagnosis |
Source: Data from ICD-10-PCS Official Guidelines for Coding and Reporting, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/PCS-2014-guidelines.pdf.
The selection of the principal procedure is not always clear-cut. Let’s go back to our case sample in which you were admitted as an inpatient and had an appendectomy to resolve your appendicitis. If, during your hospital stay, you fell out of bed and broke your hip, you might have undergone an additional surgery to repair your hip fracture. Both the appendectomy and the hip surgery meet the criteria of being performed for definitive treatment. Even though the hip repair is a more expensive procedure taking more time, the appendectomy is the principal procedure because it is most related to your principal diagnosis of appendicitis.
If more than one definitive procedure is equally related to the principal diagnosis, the most resource-intensive or complex procedure is generally designated as the principal procedure.
PCS OVERVIEW AND CONVENTIONS
This section should be used in conjunction with the ICD-10-PCS Reference Manual, which has numerous examples of PCS codes, as well as coding exercises. It is free of charge and is located at http://www.cms.gov/Medicare/Coding/ICD10/2014-ICD-10-PCS.html.
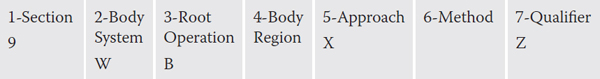
ICD-10-PCS represents a radical change from the ICD-9-CM procedure coding system being used for inpatient hospitalizations until October 1, 2015. The old system paralleled the old ICD-9-CM diagnosis coding structure; an alphabetical index was used to look up a procedure in the tabular list. With only four digits available for ICD-9-CM procedure codes, the system is severely limited in its ability to accommodate new procedures and new technology. PCS takes a new approach, in that codes are “built” using flexible components within a seven-character alphanumeric format. Each character in the code represents an aspect of the procedure, as seen in this example from the Medical and Surgical section.
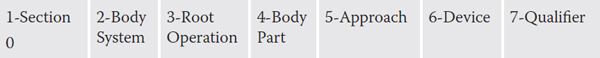
Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
One of 34 possible values can be assigned to each of the 7 characters in a procedure code. All letters may be used, with the exception of I and O, because of their potential confusion with the numbers 1 and 0. Numbers 0 through 9 are also used. Ten numbers plus 24 letters totals the 34 possible values for each character. This means that the system is almost infinitely expandable, a big improvement over ICD-9-CM.
It is important to understand that the meaning of any single value is dependent on the preceding values in the code. An example is the fourth character for body part. In the code for gastrointestinal resection, which starts with 0DT, the fourth character value of “6” is for stomach. However, in the code for resection in the respiratory system, which starts with 0BT, the fourth character of “6” is for the right lower lobe of the bronchus.
Although there is an alphabetic index in PCS, it is not mandatory to use the index first.
This represents a departure from the coding process in both the old ICD-9-CM procedure coding and the new ICD-10-CM diagnosis coding systems. The purpose of the alphabetic index in PCS is to point the coder in the direction of the correct table where all the necessary information is located to construct a valid procedure code.
Each PCS table starts with the first three defined characters. Examples include the following:
0LN |
Section: |
0 |
Medical and surgical |
|
Body system: |
L |
Tendons |
|
Root operation: |
N |
Release |
BT2 |
Section: |
B |
Imaging |
|
Body system: |
T |
Urinary system |
|
Procedure: |
2 |
CT scan |
Once the appropriate table is located, valid procedure codes must contain characters four through seven on the same line within the table. In the following table, 08D8XZZ is a valid code. However, code 08DKXZZ is not a valid code, because the value X for an external approach, which is the fifth character, is not on the same line with the fourth character (K) for left lens. Logically, this makes sense, because you cannot have an external approach to the lens because it is not on the outside of the eye.
Section: |
0 |
Medical and surgical |
Body system: |
8 |
Eye |
Root operation: |
D |
Extraction |

Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
PCS is divided into 16 sections, or broad procedural categories, with the number of valid codes in each section for 2014 as follows. Sections 0–9 are generally referred to as the medical- and surgical-related sections, whereas sections B–H are the ancillary sections. Official coding guidelines are only available for the Medical and Surgical and Obstetrics sections, with more than 86% of the total valid codes occurring in these two sections.
Character 1: Section Value |
Section Title |
Number of Valid Codes (2014) |
0 |
Medical and surgical |
61,898 |
1 |
Obstetrics |
300 |
2 |
Placement |
861 |
3 |
Administration |
1,388 |
4 |
Measurement and monitoring |
339 |
5 |
Extracorporeal assistance and performance |
41 |
6 |
Extracorporeal therapies |
42 |
7 |
Osteopathic |
100 |
8 |
Other procedures |
60 |
9 |
Chiropractic |
90 |
B |
Imaging |
2,934 |
C |
Nuclear medicine |
463 |
D |
Radiation therapy |
1,939 |
F |
Physical rehabilitation and diagnostic audiology |
1,380 |
G |
Mental health |
30 |
H |
Substance abuse treatment |
59 |
|
Total |
71,924 |
Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Medical- and Surgical-Related Sections (0–9)
MEDICAL AND SURGICAL SECTION (0)
M&S Body System Guidelines
In addition to specific body systems, such as the urinary, muscle, and respiratory systems, there are also tables with body system characters representing more general anatomical regions, such as the pelvic cavity. These should only be used when the procedure is performed on an anatomical region rather than a specific body part, such as drainage of a body cavity.
The line of reference for general body system values of “upper” and “lower” in some systems is above or below the diaphragm.
M&S Root Operations Definitions
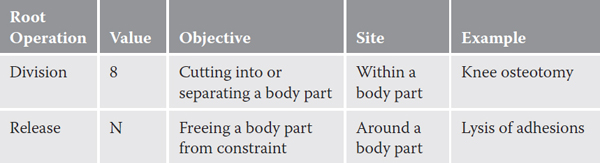
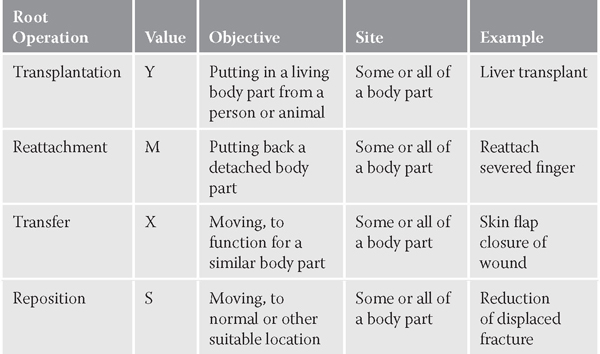
The third character in PCS medical- and surgical-related codes is the root operation. It is the answer to the question, “What is the objective of the procedure?” The root operations can be grouped by similar objectives, as follows.
Root operations that take out some or all of a body part:

Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Root operations that take out solids/fluids/gases from a body part:

Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Root operations that involve cutting or separation only:
Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Root operations that put or put back or move some or all of a body part:
Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Root operations that alter the diameter or route of a tubular body part:

Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Root operations that always involve a device:
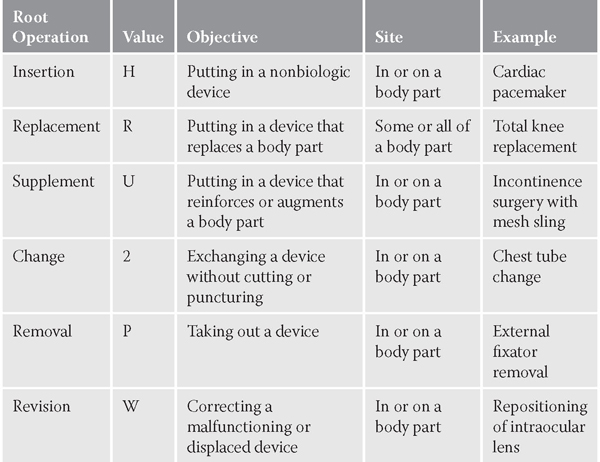
Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Root operations involving examination only:

Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Root operations that include other repairs:

Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Root operations that include other objectives:

Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
M&S Root Operation Guidelines
General guidelines:
![]() Components of a procedure specified in the root operation definition are not coded separately.
Components of a procedure specified in the root operation definition are not coded separately.
![]() Procedural steps necessary to reach and/or close the operative site are not coded separately.
Procedural steps necessary to reach and/or close the operative site are not coded separately.
Multiple procedures during the same operative episode are coded under the following circumstances:
![]() The same root operation is performed on different body parts.
The same root operation is performed on different body parts.
![]() The same root operation is repeated at different body sites that are included in the same body part value.
The same root operation is repeated at different body sites that are included in the same body part value.
![]() Multiple root operations with distinct objectives are performed on the same body part.
Multiple root operations with distinct objectives are performed on the same body part.
![]() The intended root operation is attempted using one approach but is converted to a different approach.
The intended root operation is attempted using one approach but is converted to a different approach.
Discontinued procedures:
![]() If the intended procedure is discontinued, code the procedure to whatever root operation was completed. If no other root operation was completed, code the procedure to the inspection root operation.
If the intended procedure is discontinued, code the procedure to whatever root operation was completed. If no other root operation was completed, code the procedure to the inspection root operation.
Biopsies:
![]() Biopsy procedures are coded by technique to the root operations excision, extraction, or drainage with a qualifier of diagnostic.
Biopsy procedures are coded by technique to the root operations excision, extraction, or drainage with a qualifier of diagnostic.
![]() If the biopsy procedure is followed by a more definitive procedure at the same site, both are coded.
If the biopsy procedure is followed by a more definitive procedure at the same site, both are coded.
Overlapping body layers:
![]() If the root operations excision, repair, or inspection are performed on overlapping layers of the musculoskeletal system, the body part specifying the deepest layer is used.
If the root operations excision, repair, or inspection are performed on overlapping layers of the musculoskeletal system, the body part specifying the deepest layer is used.
Bypass procedures:
![]() Bypass procedures are coded with a fourth character body part of where the bypass is from and a qualifier of the body part the bypass is to.
Bypass procedures are coded with a fourth character body part of where the bypass is from and a qualifier of the body part the bypass is to.
![]() An exception to the above is coronary arteries. They are coded according to the number of distinct sites treated, not the number of arteries. The body part is the number of artery sites bypassed to and the qualifier is the vessel bypassed from.
An exception to the above is coronary arteries. They are coded according to the number of distinct sites treated, not the number of arteries. The body part is the number of artery sites bypassed to and the qualifier is the vessel bypassed from.
![]() If multiple coronary artery sites are bypassed, each site that uses a different device and/or qualifier is coded separately.
If multiple coronary artery sites are bypassed, each site that uses a different device and/or qualifier is coded separately.
Control versus more definitive root operations:
![]() If the attempt to stop postprocedural bleeding is unsuccessful, and any of the definitive root operations is then performed, then that root operation is coded instead of control.
If the attempt to stop postprocedural bleeding is unsuccessful, and any of the definitive root operations is then performed, then that root operation is coded instead of control.
![]() Resection of a specific body part is coded whenever all of the body part is cut out or off, rather than coding a less specific body part.
Resection of a specific body part is coded whenever all of the body part is cut out or off, rather than coding a less specific body part.
Excision for graft:
![]() If an autograft is obtained from a different body part in order to complete the objective of the procedure, a separate procedure is coded.
If an autograft is obtained from a different body part in order to complete the objective of the procedure, a separate procedure is coded.
Spinal fusion procedures:
![]() At each spinal level, there are distinct body part values for single and multiple vertebral joints at each spinal level.
At each spinal level, there are distinct body part values for single and multiple vertebral joints at each spinal level.
![]() If multiple vertebral joints are fused, a separate procedure is coded for each vertebral joint that uses a different device and/or qualifier.
If multiple vertebral joints are fused, a separate procedure is coded for each vertebral joint that uses a different device and/or qualifier.
![]() When combinations of devices and materials are used on the same vertebral joint, the device value (character 6) is:
When combinations of devices and materials are used on the same vertebral joint, the device value (character 6) is:
![]() Interbody fusion device (alone or containing bone graft); code to device interbody fusion device.
Interbody fusion device (alone or containing bone graft); code to device interbody fusion device.
![]() Bone graft alone; code to device autologous or nonautologous tissue substitute.
Bone graft alone; code to device autologous or nonautologous tissue substitute.
![]() Mixture of autologous and nonautologous bone graft, with or without extenders or binders; code to autologous tissue substitute.
Mixture of autologous and nonautologous bone graft, with or without extenders or binders; code to autologous tissue substitute.
Inspection procedures:
![]() Inspection of a body part performed in order to achieve the objective of the procedure is not coded separately.
Inspection of a body part performed in order to achieve the objective of the procedure is not coded separately.
![]() If multiple tubular body parts are inspected, the most distal part is coded.
If multiple tubular body parts are inspected, the most distal part is coded.
![]() If multiple nontubular body parts in a region are inspected, the body part that specifies the entire area is coded.
If multiple nontubular body parts in a region are inspected, the body part that specifies the entire area is coded.
![]() When both an inspection procedure and another procedure are performed on the same body part during the same episode, and the inspection procedure is performed using a different approach than the other procedure, the inspection procedure is coded separately.
When both an inspection procedure and another procedure are performed on the same body part during the same episode, and the inspection procedure is performed using a different approach than the other procedure, the inspection procedure is coded separately.
Occlusion versus restriction for vessel embolization procedures:
![]() If the objective of embolization is to completely close a vessel, code to occlusion.
If the objective of embolization is to completely close a vessel, code to occlusion.
![]() If the objective is to narrow the lumen of the vessel, code to restriction.
If the objective is to narrow the lumen of the vessel, code to restriction.
Release procedures:
![]() The body part value coded is the part being freed, not the tissue being manipulated or cut to free the body part.
The body part value coded is the part being freed, not the tissue being manipulated or cut to free the body part.
![]() If the sole objective is freeing a body part without cutting it, code to release.
If the sole objective is freeing a body part without cutting it, code to release.
![]() If the sole objective is separating or transecting the body part, code to transection.
If the sole objective is separating or transecting the body part, code to transection.
Reposition for fracture treatment:
![]() Reduction of a displaced fracture is coded to reposition and any associated cast or splint application is not coded separately.
Reduction of a displaced fracture is coded to reposition and any associated cast or splint application is not coded separately.
![]() Treatment of a nondisplaced fracture is coded to the procedure performed.
Treatment of a nondisplaced fracture is coded to the procedure performed.
![]() Casting of a nondisplaced fracture is coded to immobilization in the placement section.
Casting of a nondisplaced fracture is coded to immobilization in the placement section.
Transplantation versus administration:
![]() Putting in a mature and functioning living body part taken from another individual or animal is coded to transplantation.
Putting in a mature and functioning living body part taken from another individual or animal is coded to transplantation.
![]() Putting in autologous or nonautologous cells is coded to the Administration section.
Putting in autologous or nonautologous cells is coded to the Administration section.
General:
![]() If a procedure is performed on a portion of a body part that does not have a specific value, code to the value for the whole body part.
If a procedure is performed on a portion of a body part that does not have a specific value, code to the value for the whole body part.
![]() If the prefix peri- is combined with a body part to identify the site, the procedure is coded to the body part named.
If the prefix peri- is combined with a body part to identify the site, the procedure is coded to the body part named.
Branches of body parts:
![]() If a specific branch of a body part does not have its own value, code to the closest proximal branch that does have a specific value.
If a specific branch of a body part does not have its own value, code to the closest proximal branch that does have a specific value.
Bilateral body part values:
![]() If the identical procedure is performed bilaterally and a bilateral body part value is available, code once using the bilateral body part value.
If the identical procedure is performed bilaterally and a bilateral body part value is available, code once using the bilateral body part value.
![]() If a bilateral body part value is not available, code twice using the left and right values.
If a bilateral body part value is not available, code twice using the left and right values.
Tendons, ligaments, bursae, and fascia near a joint:
![]() Procedures performed on tendons, ligaments, bursae, and fascia supporting a joint are coded to the body part in the body system that is the focus of the procedures.
Procedures performed on tendons, ligaments, bursae, and fascia supporting a joint are coded to the body part in the body system that is the focus of the procedures.
![]() Procedures performed on joint structures themselves are coded to the body part in the joint body system.
Procedures performed on joint structures themselves are coded to the body part in the joint body system.
Skin, subcutaneous tissue, and fascia overlying a joint:
![]() Procedures performed on the skin, subcutaneous tissue or fascia overlying a joint are coded to the following body parts:
Procedures performed on the skin, subcutaneous tissue or fascia overlying a joint are coded to the following body parts:
![]() Shoulder is coded to upper arm.
Shoulder is coded to upper arm.
![]() Elbow is coded to lower arm.
Elbow is coded to lower arm.
![]() Hip is coded to upper leg.
Hip is coded to upper leg.
![]() Knee is coded to lower leg.
Knee is coded to lower leg.
![]() Ankle is coded to foot.
Ankle is coded to foot.
Fingers and toes:
![]() If a body system does not contain a separate body part value for:
If a body system does not contain a separate body part value for:
![]() Fingers, code to body part value for hand.
Fingers, code to body part value for hand.
![]() Toes, code to body part value for foot.
Toes, code to body part value for foot.
Upper and lower intestinal tract:
![]() The root operations change, inspection, removal, and revision within the gastrointestinal body system contain general body part values of the following:
The root operations change, inspection, removal, and revision within the gastrointestinal body system contain general body part values of the following:
![]() Upper intestinal tract: Includes the portion from the esophagus down to and including the duodenum
Upper intestinal tract: Includes the portion from the esophagus down to and including the duodenum
![]() Lower intestinal tract: Includes the portion from the jejunum down to and including the rectum and anus
Lower intestinal tract: Includes the portion from the jejunum down to and including the rectum and anus
M&S Approach Guidelines
For the seven medical- and surgical-related sections, the fifth character is used to define the approach or technique used to reach the site of the procedure:
0 |
Open: Cutting through the skin or mucous membrane and any other body layers necessary to expose the site of the procedure |
3 |
Percutaneous: Entry, by puncture or minor incision, of instrumentation through the skin or mucous membrane and any other body layers necessary to reach the site of the procedure |
4 |
Percutaneous endoscopic: Entry, by puncture or minor incision, of instrumentation through the skin or mucous membrane and any other body layers necessary to reach and visualize the site of the procedure |
Via natural or artificial opening: Entry of instrumentation through a natural or artificial external opening to reach the site of the procedure |
|
8 |
Via natural or artificial opening endoscopic: Entry of instrumentation through a natural or artificial external opening to reach and visualize the site of the procedure |
F |
Via natural or artificial opening with percutaneous endoscopic assistance |
X |
External: Procedures performed directly on the skin or mucous membrane and procedures performed indirectly by the application of external force through the skin or mucous membrane |
Open approach with percutaneous endoscopic assistance:
![]() Procedures performed using the open approach with percutaneous endoscopic assistance are coded to the open approach.
Procedures performed using the open approach with percutaneous endoscopic assistance are coded to the open approach.
External approach:
![]() Procedures performed within an orifice on structures that are visible without the aid of any instrumentation are coded to external approach.
Procedures performed within an orifice on structures that are visible without the aid of any instrumentation are coded to external approach.
![]() Procedures performed indirectly by the application of external force through intervening body layers are coded to external approach.
Procedures performed indirectly by the application of external force through intervening body layers are coded to external approach.
Percutaneous procedure via device:
![]() Procedures performed percutaneously via a device placed for the procedure are coded to percutaneous approach.
Procedures performed percutaneously via a device placed for the procedure are coded to percutaneous approach.
M&S Device Guidelines
![]() A device is coded only if a device remains after the procedure is completed.
A device is coded only if a device remains after the procedure is completed.
![]() If no device remains, the device value of “no device” Z is used.
If no device remains, the device value of “no device” Z is used.
![]() Materials such as sutures, ligatures, radiological markers, and temporary postoperative wound drains are not coded as devices.
Materials such as sutures, ligatures, radiological markers, and temporary postoperative wound drains are not coded as devices.
![]() Procedures performed on a device only and not on a body part are coded to change, irrigation, removal, or revision.
Procedures performed on a device only and not on a body part are coded to change, irrigation, removal, or revision.
![]() A separate procedure to put in a drainage device is coded to root operation drainage with a device value of “drainage device.”
A separate procedure to put in a drainage device is coded to root operation drainage with a device value of “drainage device.”
OBSTETRICS SECTION (1)
The seven code characters retain the same meanings in the Obstetrics section.

Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Obstetrics Body Systems
The body system for this section is Pregnancy (0).
Obstetrics Root Operations
Two of the 12 root operations in the Obstetrics section are unique:
![]() Abortion (A): Artificially terminating a pregnancy
Abortion (A): Artificially terminating a pregnancy
![]() Delivery (E): Assisting the passage of the products of conception from the genital canal
Delivery (E): Assisting the passage of the products of conception from the genital canal
The other root operations available in valid obstetrics codes have the same meanings as in the Medical and Surgical section. They are the following:
![]() Change (2)
Change (2)
![]() Drainage (9)
Drainage (9)
![]() Insertion (H)
Insertion (H)
![]() Inspection (J)
Inspection (J)
![]() Repair (Q)
Repair (Q)
![]() Reposition (S)
Reposition (S)
![]() Resection (T)
Resection (T)
![]() Transplantation (Y)
Transplantation (Y)
Obstetrics Body Parts
The Obstetrics section of ICD-10-PCS includes procedures performed on the products of conception. Procedures performed on a pregnant female, other than on the products of conception, are coded to the appropriate root operation in the Medical and Surgical section (0). Thus, only three possible body part values are available in this section:
![]() Products of conception (0)
Products of conception (0)
![]() Products of conception, retained (1)
Products of conception, retained (1)
![]() Products of conception, ectopic (2)
Products of conception, ectopic (2)
Obstetrics Qualifiers
Obstetrics qualifiers include the types of C-sections, types of deliveries, types of abortifacients, fluids removed in drainage procedures on products of conception, and body systems repaired or transplanted within products of conception.
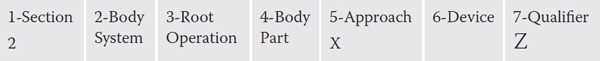
PLACEMENT SECTION (2)
The seven characters retain the same meaning in the Placement section.
Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Placement Body Systems
The Placement body systems are the following:
W |
Anatomical regions |
Y |
Anatomical orifices |
Only those procedures performed without making an incision or puncture are coded:
0 |
Change: Taking out or off a device from a body region and putting back an identical or similar device in or on the same body region without cutting or puncturing the skin or a mucous membrane |
1 |
Compression: Putting pressure on a body region |
2 |
Dressing: Putting material on a body region for protection |
3 |
Immobilization: Limiting or preventing motion of a body region |
4 |
Packing: Putting material in a body region or orifice |
5 |
Removal: Taking out or off a device from a body region |
6 |
Traction: Exerting a pulling force on a body region in a distal direction |
Placement Approach
The placement approach is always external (X).
Placement Devices
0 |
Traction apparatus |
1 |
Splint |
2 |
Cast |
3 |
Brace |
4 |
Bandage |
5 |
Packing material |
6 |
Pressure dressing |
7 |
Intermittent pressure device |
8 |
Stereotactic device |
9 |
Wire |
Y |
Other device |
Z |
No device |
The Placement qualifier is always Z, no qualifier.
ADMINISTRATION SECTION (3)
The seven characters retain the same meaning in the Administration section, except that the sixth character refers to a substance instead of a device.

Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
The codes in this section describe procedures in which a diagnostic or therapeutic substance is given to a patient.
Administration Body Systems
The codes for body systems are the following:
0 |
Circulatory |
C |
Indwelling device |
E |
Physiological systems and anatomical regions |
Administration Root Operations
0 |
Introduction: Putting in or on a therapeutic, diagnostic, nutritional, physiological, or prophylactic substance except blood or blood products |
1 |
Irrigation: Putting in or on a cleansing substance |
2 |
Transfusion: Putting in blood or blood products |
Administration Approach
All approaches are used in this section, except percutaneous endoscopic.
Substances include a wide variety of blood components, as well as substance categories such as contrast agents or local anesthetics, stem cells, and fertilized ovum.
Administration Qualifiers
Qualifiers are used to identify autologous versus nonautologous, specific drug types, and diagnostic procedures.
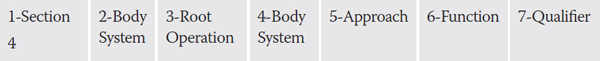
MEASUREMENT AND MONITORING SECTION (4)
The seven code characters in this system are slightly different.
Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Measurement and Monitoring Body Systems
A |
Physiological systems |
B |
Physiological devices |
Measurement and Monitoring Root Operations
0 |
Measurement: Determining the level of a physiological or physical function at a single point in time |
1 |
Monitoring: Determining the level of a physiological or physical function repetitively over a period of time |
Measurement and Monitoring Body Systems
Character 4 defines the specific system being measured or monitored.
Measurement and Monitoring Function/Device
Character 6 specifies the physiological or physical function being measured or monitored, or the device used.
0 |
Acuity |
1 |
Capacity |
2 |
Conductivity |
3 |
Contractility |
4 |
Electrical activity |
5 |
Flow |
6 |
Metabolism |
7 |
Mobility |
8 |
Motility |
9 |
Output |
B |
Pressure |
C |
Rate |
D |
Resistance |
F |
Rhythm |
G |
Secretion |
H |
Sound |
J |
Pulse |
K |
Temperature |
L |
Volume |
M |
Total activity |
N |
Sampling and pressure |
P |
Action currents |
Q |
Sleep |
R |
Saturation |
Devices
S |
Pacemaker |
T |
Defibrillator |
V |
Stimulator |
Monitoring and Measurement Qualifiers
Qualifiers are used to further define parts of various body systems.
EXTRACORPOREAL ASSISTANCE AND PERFORMANCE SECTION (5)
In this section, character 5 describes the duration of the procedure, rather than the approach.

Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Extracorporeal Assistance Body System
Only one body system, physiological systems (A), is available.
Extracorporeal Assistance Root Operations
0 |
Assistance: Taking over partial control of the physiological function. |
1 |
Performance: Taking complete control of the physiological function. |
2 |
Restoration: Returning, or attempting to return, a physiological function to its original state. Note that this applies only to external cardioversion and defibrillation. Failed cardioversion is coded the same as successful. |
Extracorporeal Body Systems
2 |
Cardiac |
5 |
Circulatory |
9 |
Respiratory |
C |
Biliary |
D |
Urinary |
Extracorporeal Duration (Character 5)
0 |
Single occurrence |
1 |
Intermittent |
2 |
Continuous |
Less than 24 consecutive hours | |
4 |
24–96 consecutive hours |
5 |
Greater than 96 consecutive hours |
6 |
Multiple occurrences |
Extracorporeal Assistance Qualifiers
The qualifiers define the type of assistance used, such as balloon pump or hyperbaric oxygenation.
EXTRACORPOREAL THERAPIES SECTION (6)
Similar to the previous section in the assignment of code characters, this section includes other extracorporeal procedures that are not defined as assistance or performance.

Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Extracorporeal Therapies Body System
The body system is physiological systems (A).
Extracorporeal Therapies Root Operations
0 |
Atmospheric control: Pressure and composition |
1 |
Decompression: Elimination of undissolved gas from body fluids |
2 |
Electromagnetic therapy: Treatment by electromagnetic rays |
3 |
Hyperthermia: Raising of body temperature |
4 |
Hypothermia: Lowering of body temperature |
5 |
Pheresis: Separation of blood products |
6 |
Phototherapy: Treatment by light rays |
7 |
Ultrasound therapy: Treatment by ultrasound |
8 |
Ultraviolet light therapy: Treatment by ultraviolet lights |
9 |
Shock wave therapy: Treatment by shock waves |
Extracorporeal Therapies Body Systems
0 |
Skin |
1 |
Urinary |
2 |
Central nervous |
3 |
Musculoskeletal |
5 |
Circulatory |
Z |
None |
Extracorporeal Therapies Duration (Character 5)
0 |
Single occurrence |
1 |
Multiple occurrences |
Extracorporeal Therapies Qualifiers
Character 6 is always value Z, none. The qualifiers in character 7 are used to indicate which blood products are separated in pheresis and which part of the circulatory system is affected in ultrasound therapy.
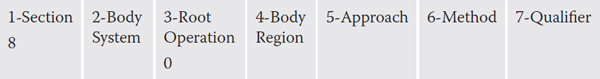
OSTEOPATHIC SECTION (7)

Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Osteopathic Body System
The system is anatomical regions (W).
Osteopathic Root Operation
The root operation is treatment (0).
Osteopathic Body Regions
0 |
Head |
1 |
Cervical |
Thoracic | |
3 |
Lumbar |
4 |
Sacrum |
5 |
Pelvis |
6 |
Lower extremities |
7 |
Upper extremities |
8 |
Rib cage |
9 |
Abdomen |
Osteopathic Approach
The approach is always external (X).
Osteopathic Methods
Methods are not defined specifically in PCS other than as follows:
0 |
Articulatory, raising |
1 |
Fascial release |
2 |
General mobilization |
3 |
High velocity, low amplitude |
4 |
Indirect |
5 |
Low velocity, high amplitude |
6 |
Lymphatic pump |
7 |
Muscle energy, isometric |
8 |
Muscle energy, isotonic |
9 |
Other method |
Osteopathic Qualifier
The qualifier is always Z, none.
OTHER PROCEDURES SECTION (8)
This section includes procedures that are not found in the other medical- and surgical-related sections.
Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Other Procedures Body Systems
C |
Indwelling device |
E |
Physiological systems and anatomical regions |
Other Procedures Root Operations
0 |
Other procedures: Methods that attempt to remediate or cure a disorder or disease |
Other Procedures Body Regions
1 |
Nervous system |
2 |
Circulatory system |
9 |
Head and neck region |
H |
Integumentary system and breast |
K |
Musculoskeletal system |
U |
Female reproductive system |
V |
Male reproductive system |
W |
Trunk region |
X |
Upper extremity |
Y |
Lower extremity |
Z |
None |
Other Procedures Methods
0 |
Acupuncture |
1 |
Therapeutic massage |
6 |
Collection |
B |
Computer-assisted procedure |
C |
Robotic-assisted procedure |
Near-infrared spectroscopy | |
Y |
Other method |
Other Procedures Approach
Standard approach definitions are used.
Other Procedures Qualifiers
Qualifiers include procedures such as suture removal, examination, piercing, plus specifics of either breastmilk or sperm for method collection, in vitro fertilization, meditation, and yoga therapy.
CHIROPRACTIC SECTION (9)
Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Chiropractic Body System
The body system is anatomical regions (W).
Chiropractic Root Operation
B |
Manipulation: Manual procedure that involves a directed thrust to move a joint past the physiological range of motion, without exceeding the anatomical limit |
Chiropractic Body Regions
0 |
Head |
1 |
Cervical |
2 |
Thoracic |
3 |
Lumbar |
4 |
Sacrum |
5 |
Pelvis |
6 |
Lower extremities |
Upper extremities | |
8 |
Rib cage |
9 |
Abdomen |
Chiropractic Approach
The approach is always external (X).
Chiropractic Methods
Methods are not defined within PCS, except as follows:
B |
Nonmanual |
C |
Indirect visceral |
D |
Extra-articular |
F |
Direct visceral |
G |
Long lever specific contact |
H |
Short lever specific contact |
J |
Long and short level specific contact |
K |
Mechanically assisted |
L |
Other method |
Chiropractic Qualifier
The qualifier is always Z, none.
Ancillary Sections (B–D and F–H)
The six ancillary sections all use a third coding character called “root type,” instead of root operation. It defines the type of procedure performed. Characters 4, 5, and 6 also have different definitions, as described in the following sections.
IMAGING SECTION (B)

Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Many values are possible, similar to the Medical and Surgical section.
Imaging Root Types
Root type describes the category of procedure performed:
0 |
Plane radiography: Planar display of an image developed from the capture of external ionizing radiation on photographic or photoconductive plate |
1 |
Fluoroscopy: Single plane or bi-plane real-time display of an image developed from the capture of external ionizing radiation on a fluorescent screen |
2 |
CT scan: Computer reformatted digital display of multiplanar images developed from the capture of multiple exposures of external ionizing radiation |
3 |
MRI: Computer reformatted digital display of multiplanar images developed from the capture of radio frequency signals emitted by nuclei in a body site excited within a magnetic field |
4 |
Ultrasonography: Real-time display of images of anatomy or flow information developed from the capture of reflected and attenuated high-frequency sound waves |
Imaging Body Parts
Defines more specifically the part of the body system from character 2.
Imaging Contrast
0 |
High osmolar |
1 |
Low osmolar |
Y |
Other contrast |
Z |
None |
Imaging Qualifier (Character 6)
Many tables contain a value of Z, none, for character 6, but in a few cases it is used to provide more detail about technique, such as with and without contrast, identified as unenhanced and enhanced.
Imaging Qualifier (Character 7)
Character 7 usually has a value of Z, none, but a few tables have entries such as intraoperative, guidance, or other descriptive enhancements.
NUCLEAR MEDICINE SECTION (C)
This section is very similar to the Imaging section, except that character 5 is used to describe the radionuclide, or radiation source, used in the procedure.

Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Nuclear Medicine Body Systems
Many options are available, similar to the Medical and Surgical section.
Nuclear Medicine Root Types
1 |
Planar nuclear imaging: Introduction of radioactive materials into the body for single-plane display of images developed from the capture of radioactive emissions |
2 |
Tomographic (tomo) nuclear medicine imaging: Introduction of radioactive materials into the body for three-dimensional display of images developed from the capture of radioactive emissions |
3 |
Positron emission tomographic (PET) imaging: Introduction of radioactive materials into the body for three-dimensional display of images developed from the simultaneous capture, 180 degrees apart, of radioactive emissions |
Nonimaging nuclear medicine uptake: Introduction of radioactive materials into the body for measurements of organ function, from the detection of radioactive emissions | |
5 |
Nonimaging nuclear medicine probe: Introduction of radioactive materials into the body for the study of distribution and fate of certain substances by the detection of radioactive emissions from an external source |
6 |
Nonimaging nuclear medicine assay: Introduction of radioactive materials into the body for the study of body fluids and blood elements, by the detection of radioactive emissions |
7 |
Systemic nuclear medicine therapy: Introduction of unsealed radioactive materials into the body for treatment |
Nuclear Medicine Body Parts
Many options are available to further define the body system in character 2.
Nuclear Medicine Radionuclide
Many options are available to define the actual element used, such as cobalt-58 or gallium-67.
Nuclear Medicine Qualifiers (Characters 6 and 7)
The qualifiers are always Z, none.
RADIATION THERAPY SECTION (D)
Defines the procedures used for radiation treatment of cancer.

Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Radiation Therapy Body Systems
Many options are available, similar to the Medical and Surgical section.
The root type defines the modality used in radiation therapy:
0 |
Beam radiation |
1 |
Brachytherapy |
2 |
Stereotactic radiosurgery |
Y |
Other radiation |
Radiation Therapy Body Part
Defines the specific area that the radiation therapy is focused on.
Radiation Therapy Modality Qualifier
The qualifier further defines the therapy given, using terms such as hyperthermia, photons, electrons, and neutrons.
Radiation Therapy Isotope
Defines the specific radioactive material used in therapy, such as cesium-137 or strontium-90.
Radiation Therapy Qualifier
The therapy qualifier is either intraoperative (0) or none (Z).
PHYSICAL REHABILITATION AND DIAGNOSTIC AUDIOLOGY SECTION (F)

Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Rehab and Audiology Section Qualifier (Character 2)
In this section, character 2 is known as a section qualifier. It merely defines which type of treatment is being provided:
0 |
Rehabilitation |
1 |
Diagnostic audiology |
Rehab and Audiology Root Types
Assessment Determination of the patient’s diagnosis when appropriate, need for treatment, planning for treatment, periodic assessment and documentation related to the following activities:
0 |
Speech assessment |
1 |
Motor and/or nerve function assessment |
2 |
Activities of daily living assessment |
3 |
Hearing assessment |
4 |
Hearing aid assessment: Appropriateness and/or effectiveness |
5 |
Vestibular assessment |
Treatment Use of specific activities or methods to develop, improve, and/or restore the performance of necessary functions, compensate for dysfunction, and/or minimize debilitation:
6 |
Speech treatment: Improve, augment, or compensate for impairment |
7 |
Motor treatment |
8 |
Activities of daily living treatment |
9 |
Hearing treatment |
B |
Cochlear implant treatment |
C |
Vestibular treatment |
Fitting Design, fabrication, modification, selection, and/or application of splint, orthosis, prosthesis, hearing aids, and/or other rehabilitation device:
D |
Device fitting |
Caregiver Training Educating caregiver with the skills and knowledge used to support the patient’s optimal level of function:
F |
Caregiver training |
Rehab and Audiology Body System and Region
Many options are possible.
Rehab and Audiology Type Qualifier (Character 5)
More than 100 different tests or methods for assessments and types of training are available.
Rehab and Audiology Equipment (Character 6)
Many types of equipment can be coded, such as audiometer, sound booth, prosthesis, and cochlear implant.
Rehab and Audiology Qualifier (Character 7)
Character 7 is always Z, none.
MENTAL HEALTH SECTION (G)
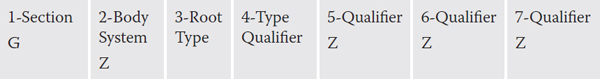
Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
This section is not as specific as many others, because it uses only three of the seven available characters. The Body System and Qualifier fields are not used and are always value Z, none.
Mental Health Root Types
Codes for the procedure performed:
1 |
Psychological tests: The administration and interpretation of psychological tests and measurement instruments for the assessment of psychological function |
2 |
Crisis intervention: Treatment of a traumatized, acutely disturbed, or distressed individual for the purpose of short-term stabilization |
3 |
Medication management: Monitoring and adjusting the use of medications for treatment of a mental health disorder |
Individual psychotherapy: Treatment of an individual with a mental health disorder by behavioral, cognitive, psychoanalytic, psychodynamic, or psychophysiological means to improve functioning or well-being | |
6 |
Counseling: The application of psychological methods to treat an individual with normal developmental issues and psychological problems in order to increase function, improve well-being, alleviate distress, address maladjustment, or to resolve crises |
7 |
Family psychotherapy: Treatment that includes one or more family members of an individual with a mental health disorder by behavioral, cognitive, psychoanalytic, psychodynamic, or psychophysiological means to improve functioning or well-being |
B |
Electroconvulsive therapy: The application of controlled electrical voltages to treat a mental health disorder |
C |
Biofeedback: Provision of information from the monitoring and regulating of physiological processes in conjunction with cognitive-behavioral techniques to improve patient functioning or well-being |
F |
Hypnosis: Induction of a state of heightened suggestibility by auditory, visual, or tactile techniques to elicit an emotional or behavioral response |
G |
Narcosynthesis: Administration of intravenous barbiturates in order to release suppressed or repressed thoughts |
H |
Group psychotherapy: Treatment of two or more individuals with a mental health disorder by behavioral, cognitive, psychoanalytic, psychodynamic, or psychophysiological means to improve functioning or well-being |
J |
Light therapy: Application of specialized light treatments to improve functioning or well-being |
Mental Health Type Qualifier (Character 4)
The qualifier further defines the type of therapy, test, or treatment, as appropriate to the root type procedure.
SUBSTANCE ABUSE TREATMENT SECTION (H)
This is another section that only uses three characters in building codes.

Source: Data from ICD-10-PCS Reference Manual, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/Downloads/2014-Reference-Manual.zip.
Substance Abuse Root Types
2 |
Detoxification services: Detoxification from alcohol and/or drugs |
3 |
Individual counseling: The application of psychological methods to treat an individual with addictive behavior |
4 |
Group counseling: The application of psychological methods to treat two or more individuals with addictive behavior |
5 |
Individual psychotherapy: Treatment of an individual with addictive behavior by behavioral, cognitive, psychoanalytic, psychodynamic, or psychophysiological means |
6 |
Family counseling: The application of psychological methods that includes one or more family members of an individual with addictive behavior |
8 |
Medication management: Monitoring and adjusting the use of replacement medications for the treatment of addiction |
9 |
Pharmacotherapy: The use of replacement medications for treatment of addiction |
Substance Abuse Type Qualifier (Character 4)
This qualifier further defines the type of therapy, pharmacotherapy, or counseling.
The ICD-10-PCS Reference Manual includes a body part key that can be helpful in determining which body part should be used for a specific anatomic structure. For example, the term “lesser trochanter” will not be found in the section table. If that term is located in the body part key, it indicates that the body part of upper femur, left or right, should be used in building the code. Likewise, the device key provides a crosswalk from brand-name devices to the appropriate device category, such as specifying that “Wallstent© endoprosthesis” is in the intraluminal device category.
PCS Coding Challenges
The ability to assign the correct ICD-10-PCS code to a documented procedure relies heavily on three types of coder knowledge (Rousse, 2013):
1. Foundational knowledge: Knowledge of medical terminology, anatomy and physiology, and pathophysiology
2. Conceptual knowledge: Familiarity with official coding guidelines, root operation definitions, the body part key, and the device key
3. Interpretive knowledge: The ability to use critical thinking to translate clinical documentation into appropriate root operations
The Official Guidelines for Coding and Reporting (CMS, 2014c) state:
Many of the terms used to construct PCS codes are defined within the system. It is the coder’s responsibility to determine what the documentation in the medical record equates to in the PCS definitions. The physician is not expected to use the terms used in PCS code descriptions, nor is the coder required to query the physician when the correlation between the documentation and the defined PCS terms is clear. (Convention A.11)
The real issue, then, is how often the correlation is not clear. The process of learning medical terminology involves prefix and suffix meanings. In the old coding system, -ectomy generally meant “excision.” Now -ectomy can mean either “root operation excision” or “root operation resection,” depending on what and how much was removed.
Some of the root operation terms are unusual, such as extirpation and detachment. Some commonly used terms, such as amputation, are not root operations in PCS. There is little correlation between the terminology in PCS and that found in CPT, which physicians continue to use for their own billing. Because physicians are not expected to use PCS terms, they continue to use their own familiar terminology, including eponyms such as Whipple procedure or McBride bunionectomy. The coder, who might previously have assigned codes based solely on the documented name of the procedure, now has to read the description of the surgical technique and code what was actually done. Additional code characters use details usually not considered under the old system, such as laterality and approach. Devices and substances were also not coded as specifically.
Computer-assisted coding (CAC) uses natural-language processing to “read” reports, identify relevant codeable terms, and suggest codes to the coder, who then makes the final determination of the correct code assignment. A study conducted by the AHIMA Foundation found that the use of CAC resulted in a 22% reduction in the amount of coding time per record and did not result in reduced accuracy when used by a credentialed coder (Dougherty, Seabold, & White, 2013). PCS is an elegant system in its structure and expandability, but it is a labor-intensive system. CAC technology can be used to make up for some of the coder productivity declines inherent in PCS use.
For all medical and surgical services other than hospital inpatient, the CPT (Current Procedural Terminology) code consists of five numbers representing a unique service. The classification structure is divided into six main sections:
![]() Anesthesia (00100 to 01999)
Anesthesia (00100 to 01999)
![]() Surgery (10021 to 69990)
Surgery (10021 to 69990)
![]() Radiology (70010 to 79999)
Radiology (70010 to 79999)
![]() Pathology and Laboratory (80047 to 89399)
Pathology and Laboratory (80047 to 89399)
![]() Medicine (90281 to 99607)
Medicine (90281 to 99607)
![]() Evaluation and Management (99201 to 99499)
Evaluation and Management (99201 to 99499)
Despite the fact that the system is divided into categories, a CPT code from any category may be used by any physician or surgeon, regardless of specialty. The Evaluation and Management section is used by all specialties and represents some of the most frequently billed services. Code 99213, which is an expanded office visit for an established patient, was the number one CPT procedure code submitted to Medicare in 2011, with more than 100 million visits totaling more than $6.7 billion in allowed charges (CMS, n.d.).
The index to CPT is organized alphabetically and includes main terms that may denote a procedure or service, an organ or anatomic site, a condition, or synonyms, eponyms, or abbreviations. When searching the index, if a listing is not found under what appears to be the main term, search under one of the other words in the procedure description. Once a main term has been located, review the subterms below it to determine which is the most appropriate, given the description of the procedure that was performed.
Unlike ICD-10-PCS procedure coding, no official national rules govern the use of CPT. However, CPT codes can also be a determinant in reimbursement, thus various governmental agencies have developed their own guidelines to ensure consistency and conformity to coding definitions. Each section of CPT itself also has instructions applicable to that section.
If the CPT definition of a code includes a defined time period, there must be documentation from the physician indicating how much time he or she spent performing the service. An example of this would be 90804, which is “Individual psychotherapy, insight oriented, behavior modifying and/or supportive, in an office or outpatient facility, approximately 20 to 30 minutes face-to-face with the patient.” Codes with the time specified in the definition are known as “time-based” codes.
Sometimes there is no existing CPT code that adequately describes the procedure performed. This may be due to new techniques, additional technological developments, or procedures performed on anomalous anatomy caused by congenital malformations. Each section of CPT has an “unlisted” code, usually ending in “99,” that is to be used in this situation. It is important to note that the presence of a code in CPT describing a service does not mean that a specific third-party payer will reimburse for that service.
CPT Modifiers
An additional feature of CPT is the use of “modifiers” to indicate that specific circumstances have changed the performed service. An example would be the use of modifier -50 to indicate that a procedure not already defined as bilateral was performed on both sides of the body at the same episode of care. Modifiers play a key role in explaining to payers why procedures that look like they should not be paid separately are in fact justified. Modifiers that affect pricing or payment should be placed in the first position after the procedure code on the claim to ensure correct processing.
Some of the most commonly used HCPCS modifiers are (“Fact Sheets on CPT Modifiers,” n.d.) the following:
Increased procedural service, which is service greater than that usually required. This could occur if, for example, a surgeon is operating on a patient who is grossly obese. It takes more work to cut through additional tissue. |
|
24 |
Unrelated evaluation and management (E&M) service by the same physician or other qualified healthcare professional during a postoperative period. If you fall and break your ankle and have a surgical repair, there is a 90-day global period after the surgery where follow-ups are included in the charge for the surgery. If you fall and break your wrist during that time and go to the same doctor, he would use a -24 modifier on your wrist-related office visit to tell the payer it is unrelated to the previous surgery. |
25 |
Two procedures performed during the same episode of care: one was an E&M service, such as an office visit, and the other was a procedure. Normally, the visit would be included in the charge for the procedure, but if there is significant separate documentation of the E&M the use of both procedure codes could be justified. This situation often occurs when a patient comes in for an office visit for ongoing medical conditions, such as hypertension, and then has another problem that requires a procedure, such as removing a wart. |
26 |
Professional component of a service. Many procedures have a professional component and a technical component. An example is a chest X-ray. The technical component consists of the equipment used to do the X-ray, the salary of technician who performs the exam, and the costs of supplies, such as films. The professional component is for the physician who interprets the films and documents his findings. (This is a pricing modifier and thus should be listed first.) |
A procedure that was performed bilaterally. It can only be used for procedures that can anatomically be bilateral. For example, a bladder procedure could not be bilateral because you only have one bladder. Some CPT codes already indicate that the procedure is bilateral, such as 58605, ligation or transection, fallopian tube(s), unilateral or bilateral. This code would be used for all operations of this type, whether unilateral or bilateral. It would not be appropriate to add a -50 modifier to this code for a bilateral procedure. |
|
52 |
A service partially reduced or eliminated at the discretion of the physician. This could include a time-based procedure that is not performed for the entire time specified in the code description. |
53 |
Surgical procedure terminated after the start of anesthesia, due to extenuating circumstances, for the well-being of the patient. This modifier is used only for physician professional services; it is not used for hospital facility outpatient billing. (This is a pricing modifier and thus should be listed first.) |
54 |
Surgeon is billing for surgical care only and others are providing the preoperative and postoperative care in the global surgical period. |
57 |
Decision for surgery. For example, this modifier can be used by the surgeon who performed your appendectomy in order to bill for the visit during which he decided that you needed surgery. If the visit and the surgery occur on the same calendar date, the payer would normally consider the visit to be part of the surgical package. Using the modifier -57 on the visit code tells the payer that the surgeon did not make the decision to do surgery until that day. Obviously, this modifier cannot be used with elective, scheduled procedures. |
58 |
A staged or related procedure during the postoperative period. This would denote a procedure that was planned at the time of the original procedure, more extensive than the original procedure, or a therapeutic procedure following a diagnostic surgical procedure. If the second procedure is for a complication of the first and a return trip to the operating room is required, then modifier -78 is used instead. |
A procedure was distinct or separate from other procedures performed on the same date. Let’s assume that you had two skin lesions, one on each arm, that are excised by a dermatologist. Because the skin is considered to be a single organ covering the entire body, these cannot be coded as bilateral procedures. It would be appropriate to code the first excision and then code the second with a -59 modifier to indicate the separate site. This tells the insurance company that the doctor is not inadvertently submitting a duplicate procedure. The -59 can be used for a different site, a separate lesion or injury, a different operative session, or a different patient encounter. |
|
62 |
Co-surgeons jointly performing a single procedure. Each surgeon bills the same code with a -62 modifier. Payment to each is usually 62.5% of the normal amount. (Note that this is a pricing modifier and thus should be listed first.) |
73 |
An ambulatory surgery center (ASC) discontinued a procedure prior to the administration of anesthesia. This modifier is used by ASCs to demonstrate use of their resources when the patient is prepared for surgery and taken to the room where the procedure is to be performed but the procedure is canceled before anesthesia has been administered. This could happen if the patient’s blood pressure is too high, if new lab results reveal contraindications to surgery, or other reasons. If a procedure is cancelled before the patient goes to the procedure room, the procedure is not reported at all. |
74 |
This is the ASC equivalent of modifier -53 used by physicians. It identifies procedures that are discontinued after the administration of anesthesia. If more than one procedure was planned, and one or more completed, the completed procedure(s) would be reported without the modifier. It should only be used if none of the procedures were fully completed. |
A repeat procedure by the same physician or other qualified healthcare professional. It is used to note the same exact procedure, same site, same provider, and same date. This modifier is often used with radiological procedures performed more than once on a date, as required by the patient’s condition. Another example would be multiple EKGs to monitor a patient’s heart condition. |
|
77 |
A repeat procedure by another physician. It is used to note the same exact procedure, same site, same date, but different doctor. It is just like modifier -76, but a different physician performed the second or subsequent procedure. Not used with E&M services. |
78 |
Return to the operating room for a related procedure during the postoperative period. This modifier is often used when complications of the original procedure require an additional procedure. |
79 |
Unrelated procedure or service by the same physician during the postoperative period. This is the surgical equivalent of modifier -24. |
80 |
Assistant surgeon. This doctor bills the same code as the surgeon but adds an -80 modifier. |
91 |
Repeat clinical lab. Used when multiple results are necessary in the course of treatment on the same date. Should not be used for repeats due to equipment failure or inadequate specimens. If the second test is performed on a specimen from a different site, modifier -59 should be used instead of modifier -91. |
Many other modifiers also are available. For example, anesthesia modifiers identify the type of provider and supervision. Anatomical modifiers are available to identity fingers, toes, eyelids, and coronary arteries. Situational modifiers are also available for ambulance services, mammography, durable medical equipment (DME), and orthotics and prosthetics. Different payers may have different rules about which modifiers are valid in various service locations.
Additional CPT Coding Guidelines
Each section of CPT has coding guidelines to direct the use of the codes in that section.
ANESTHESIA
The services in this section include pre- and postoperative visits, anesthesia care during the procedure, fluid or blood administration, and standard monitoring of vital signs, heart rate, and rhythm. In addition, there is an official definition of anesthesia time, which “begins when the anesthesiologist begins to prepare the patient for the induction of anesthesia in the operating room or an equivalent area and ends when the anesthesiologist is no longer in personal attendance, that is, when the patient may be safely placed under post-operative supervision” (AMA, 2014).
Each anesthesia case also has an indicator of how sick the patient was. Some payers will increase the amount of reimbursement for sicker patients (“Anesthesia Physical Status Modifiers,” 2013):
P1 |
Normal healthy patient |
P2 |
Patient with mild systemic disease |
P3 |
Patient with severe systemic disease |
P4 |
Patient with severe systemic disease that is a constant threat to life |
P5 |
Moribund patient who is not expected to survive without the operation |
P6 |
Brain-dead patient whose organs are being removed for donor purposes |
Separate codes also are available to denote patients younger than age 1 or older than age 70, emergency anesthesia, and the use of total body hypothermia or controlled hypotension.
SURGERY
Codes in this section always include the following services in what is known as a “surgical package.” This means that these services should not be billed in addition to the code for the surgical procedure (AMA, 2014):
![]() Local infiltration, metacarpal/metatarsal/digital block, or topical anesthesia
Local infiltration, metacarpal/metatarsal/digital block, or topical anesthesia
![]() One related evaluation and management encounter on the day before or the day of surgery (apart from the decision for surgery)
One related evaluation and management encounter on the day before or the day of surgery (apart from the decision for surgery)
![]() Immediate postoperative care, such as talking with the patient’s family, dictating the operative report, and so on
Immediate postoperative care, such as talking with the patient’s family, dictating the operative report, and so on
![]() Writing orders
Writing orders
![]() Evaluating the patient in the postanesthesia recovery unit
Evaluating the patient in the postanesthesia recovery unit
![]() Typical post-op follow-up care
Typical post-op follow-up care
The time frame for the surgical package, or “global period,” is related to the seriousness of the surgery and the length of time needed for follow-up. The standard periods are the following:
![]() 0 days: day of surgery only
0 days: day of surgery only
![]() 10 days: day of surgery and 10 days after (11 days total)
10 days: day of surgery and 10 days after (11 days total)
![]() 90 days: day before surgery, day of surgery, and 90 days after (92 days total)
90 days: day before surgery, day of surgery, and 90 days after (92 days total)
Care for complications or unrelated problems is not included and could be billed separately during the global period using the modifiers described earlier to indicate the situation.
Surgical coding is based on the documentation in the patient’s medical record. For procedures that are performed in an operating room, the surgeon prepares an operative report in which he describes the procedures performed, the type of anesthesia used, the techniques employed, specimens removed, estimated blood loss, pre- and postoperative diagnoses, the names of the surgeon and any assistants, and whether any complications occurred.
Some of the procedure categories in the surgery section are coded using methods requiring precise measurements. For example, skin lesion removal is categorized according to the method of removal, without regard to whether the lesion is benign or malignant (cancerous), and the size of the lesion. In the case of cancerous lesions, the margin of surrounding skin that is removed is also counted. If the physician does not document all of this, the coder has to rely on the measurements in the pathology report, which may be smaller due to shrinkage of the specimen. Suturing of wound repairs also relies on size. In this type of coding, the lengths of wounds repaired in the same manner in the same anatomic group are added together to get the final measurement and code.
In the musculoskeletal category, one must be mindful of the fact that fracture treatment (open or closed) can be confused with the type of fracture (open or closed). It is possible to perform an open treatment of a closed fracture. Open treatment refers to surgical opening of the fracture site; internal fixation devices may be used to treat the fracture.
Many procedures are now performed endoscopically. A surgical endoscopy always includes a diagnostic endoscopy. It may be appropriate to use more than one code for an endoscopy if more than one procedure is performed during the same session, such as removal of foreign body, biopsy, snare, dilation, or control of bleeding.
An oft-used category in the Surgery section is Maternity Care and Delivery. Obstetrics, like surgery, has a global package of services:
![]() Antepartum care: monthly visits up to 28 weeks, biweekly visits to 36 weeks, and weekly visits until delivery.
Antepartum care: monthly visits up to 28 weeks, biweekly visits to 36 weeks, and weekly visits until delivery.
![]() Delivery: admission to the hospital, management of uncomplicated labor, vaginal or cesarean delivery.
Delivery: admission to the hospital, management of uncomplicated labor, vaginal or cesarean delivery.
![]() Postpartum care: hospital and office visits following delivery.
Postpartum care: hospital and office visits following delivery.
RADIOLOGY
Some radiologic procedures are coded using what is known as “component coding.” This occurs when part of the procedure is actually a surgical procedure, whereas the other part is the supervision and interpretation by the radiologist. An example is a knee arthrogram, which is an X-ray study of the knee joint after the injection of contrast media, which makes the details of the joint more visible. In this case, there is one code for the injection and a second code for the radiological supervision and interpretation of the films. If the radiologist does both procedures, he gets to bill both. If an orthopedist does the injection, then the radiologist only bills for the supervision and interpretation. The separate code for injection of contrast is not used if the code description for a CT, an MRA, or an MRI defines a procedure as being “with contrast.” An example is 73701, which is defined as “computed tomography, lower extremity, with contrast material.”
Component coding is also used in interventional radiology, in which catheters may be threaded through blood vessels to treat conditions located far from the point of entry. An example would be inserting a catheter into an artery in the leg and maneuvering it through the body to the location of an aneurysm (i.e., a weak spot in the wall of a blood vessel), possibly in the brain. A detachable coil is passed through the catheter and left at the aneurysm site. The body reacts to the coil by forming a blood clot around it, thus strengthening the wall of the blood vessel. Interventional radiology coding requires extensive knowledge of anatomy as well as thorough documentation by the radiologist of the entry site, all vessels imaged, and any contrast injections performed.
Radiation oncology and radiopharmaceutical therapy are also part of this section. They include codes for various types of radiation or radiopharmacy therapy for cancer. In addition to the actual treatments themselves, codes are available for clinical treatment planning, which involves localization of the tumor, measurement of the patient’s body contour, and calculation of the optimum treatment sequences to treat the diseased area while protecting other organs from adverse effects of radiation.
Mammography is a frequently performed radiologic procedure. Screening mammograms are performed on a regular basis as a preventive measure in the identification of breast cancer. If a patient has abnormal findings, a diagnostic mammogram may be done.
PATHOLOGY AND LABORATORY
This section is challenging to coding analysts because of the variety of personnel involved in laboratory testing and because of the use of “panels” to lump certain groups of tests together. Some laboratory procedures are performed by physicians, whereas others are performed by technicians under the supervision of a physician.
Surgical pathology involves the gross and microscopic exam of different types of tissue that were removed at surgery. The gross exam is the appearance of the specimen to the eyes of the pathologist; the microscopic exam is the examination of portions of the tissue specimen under a microscope. An autopsy is similar to surgical pathology except that it is the examination of the body after death. It is performed to determine the cause of death or to verify the diagnosis.
MEDICINE
Services in this section are primarily diagnostic procedures from a variety of specialties, including some that would normally be thought of as surgical, not medical, such as ophthalmology (eye) and otorhinolaryngology (ear, nose, and throat). Psychiatry is one of the specialties covered in this section. Many of the codes in the psychiatry section are time-based codes.
CPT also contains a few codes for services thought of as alternative therapies, such as acupuncture. Practitioners who use alternative treatments have initiated their own code set, known as Alternative Billing Codes (ABC) codes, which are authorized under HIPAA as acceptable for internal, statistical, and cash transactions, but are not yet part of the official code set recognized under HIPAA for third-party billing (“ABC Codes Explained,” n.d.).
EVALUATION AND MANAGEMENT (E&M)
Last in numerical order, but certainly not last in terms of utilization for billing purposes, the Evaluation and Management (E&M) section is probably the least understood and most controversial. Prior to 1992, this section occupied only four pages in CPT. The coding system for office visits was simple, based on four levels of visits.
The year 1991 was busy in the healthcare coding world. The predecessor of the CMS, the Health Care Financing Administration (HCFA), implemented a new fee schedule for Medicare services. It was based on a system known as RBRVS, or the Resource-Based Relative Value Scale. The system assigned relative-value units to each CPT code, based on physician work effort, practice expense, and malpractice insurance expense. The system was an effort to move away from the previous “usual and customary” method of calculating fees based on prevailing charges that was faulted for driving up the cost of health care.
The RBRVS also recognized that the cognitive efforts expended by primary care providers such as internists, family practitioners, and pediatricians needed to be more highly valued in comparison to surgical services. A new scheme for coding office visits and other E&M services was implemented in 1992. The instructions and guidelines for these services now occupy 44 pages in CPT, compared with 4 pages prior to 1991 (Nirschl, 2001). The medical profession was not happy with these new codes because they required substantial amounts of additional documentation. Many practitioners felt they had to document items that were not essential to patient care in order to justify their billing.
Currently, two sets of E&M documentation guidelines issued by Medicare are in use: 1995 and 1997. Physicians may use either set. A draft revision of the guidelines was released in 2000, and CMS contracted with a private firm to develop clinical vignettes to provide guidance on coding for various medical specialties. The 2000 guidelines were never implemented. In fact, the Health and Human Services Advisory Committee on Regulatory Reform voted in 2002 to abolish the E&M guidelines.
Put bluntly, physicians do not like these codes. They are extremely complex and difficult to interpret. In studies where physicians and coding analysts assigned E&M codes to hypothetical cases, the coding analysts agreed with expert opinion only 57% of the time (King, Lipsky, & Sharp, 2002), whereas agreement by physicians was only 52% (King, Sharp, & Lipsky, 2001). This indicates a lot of gray areas in coding these services.
The three key components of an E&M service are history, exam, and medical decision making. These are the components that the physician must tally when arriving at an overall level for the E&M service. For example, a Level 4 established patient office visit (99214), for which Medicare will reimburse about $115 in Oklahoma ($145 in New York City), requires a detailed history, a detailed exam, and moderately complex decision making. To document this level of care and justify the claim to the payer, the doctor will have to document the following:
![]() At least four elements of the history of present illness
At least four elements of the history of present illness
![]() Review of two to nine systems
Review of two to nine systems
![]() At least one part of the past, family, or social history
At least one part of the past, family, or social history
![]() Examination of five to seven body areas or systems
Examination of five to seven body areas or systems
![]() Review of three types of data
Review of three types of data
![]() Presence of existing problems that are worsening or new problems that may or may not require additional workup
Presence of existing problems that are worsening or new problems that may or may not require additional workup
![]() Risks of treatment options or procedures proposed
Risks of treatment options or procedures proposed
The AMA has defined the average amount of time for this level of visit as 25 minutes. If your doctor spends 25 minutes with you and more than half of that time is spent on counseling and coordination of care, such as talking with you about test results, treatment options, prognosis and risk factors, the doctor can bill for a Level 4 visit without documenting all of the key component items just listed. He merely has to state, “I spent more than 50% of this 25-minute visit discussing [topic of discussion] with the patient.”
If we assume that the physician works a 10-hour day, with an hour for lunch, he has a total of 540 minutes to see patients. He can accommodate 21 patients at 25 minutes apiece if he bills based on the amount of time he spends talking with you. Or, he can adopt methods that allow him to document all of the required pieces more quickly in order to get the same level of payment in fewer minutes. Using the latter approach, he could conceivably double the number of patients seen, thus doubling his reimbursement. This is legitimate, assuming that all the necessary documentation is present in your medical record and all the visits were medically necessary. An argument could be made that the E&M system rewards documentation and not face-to-face patient care.
The following is the process for assigning an E&M code:
![]() Determine the location (place of service) where the E&M service was performed
Determine the location (place of service) where the E&M service was performed
![]() Select the appropriate category of E&M code based on the location
Select the appropriate category of E&M code based on the location
![]() Score the documentation counting the elements of the key components (history, exam, medical decision making) or using the counseling and coordination of care option
Score the documentation counting the elements of the key components (history, exam, medical decision making) or using the counseling and coordination of care option
Under normal circumstances, a physician may only bill one E&M service per patient per day. If your doctor sees you in his office and decides that you are so sick you need to be admitted to the hospital and then stops by the hospital later that day to see you, he must “roll up” the office services into the code for the initial inpatient hospital care. Likewise, if you go to the emergency room and the ER physician decides you need to be observed for a period of time to monitor your condition, he may place you in observation status. The emergency room service must be “rolled up” into the observation service code for that date. Exceptions to the rule of one E&M per day would need to be justified through the use of modifiers indicating the circumstance.
Critical care in CPT terms does not occur just because you are in a critical care unit. Sometimes patients in those units may be there because they are awaiting a bed elsewhere in the hospital, awaiting the completion of discharge or transfer arrangements, or other administrative reasons. In order to meet the CPT definition of critical care, the patient must be critically ill or injured to the extent that one or more vital organ system is impaired and there is a high probability of imminent or life-threatening deterioration in his or her condition. In addition, the service provided must involve highly complex medical decision making to assess, manipulate, and support single or multiple vital organ system failure or prevent further life-threatening deterioration of the patient’s condition (AMA, 2014).
CPT codes for adult critical care are time based: for the first 30 minutes (or less), and then for each additional 30 minutes. Physicians must clearly document their time on adult critical care. For children 71 months of age or younger, the neonatal and pediatric critical care codes are “per day” codes, which means that all critical care services that date are included.
Procedure Coding Summarized
In this chapter, you have learned that procedure coding depends on the location where the service is provided and the type of charge being coded.
|
Hospital Inpatients |
All Others |
Facility Bill |
ICD-10-PCS procedure codes (as of October 1, 2015) |
CPT / HCPCS procedure codes |
Physician Bill |
CPT / HCPCS procedure codes |
CPT / HCPCS procedure codes |
Procedure coding also depends, ultimately, on the physician’s documentation in the medical record. The physician may know that he or she performed a procedure, but if it isn’t documented, it wasn’t done, as far as the coder is concerned.
The CPT Editorial Panel, in conjunction with medical and surgical specialty societies, receives and reviews suggestions for changes to CPT. CPT codes are updated annually, effective on January 1st. When codes change, the date of service of the procedure determines whether an old or new code is appropriate. It is imperative that the current version of CPT be used for coding and payment purposes.
References
ABC codes explained. (n.d.). Retrieved March 23, 2014, from http://www.abccodes.com/ali/abc_codes/
American Medical Association. (2014). Current procedural terminology 2014. Chicago, IL: AMA Press.
Anesthesia physical status modifiers fact sheet. (2013, April). WPS Health Insurance website. Retrieved January 22, 2014, from http://wpsmedicare.com/j5macpartb/resources/modifiers/modifier-anes-physstatus.shtml
Centers for Medicare and Medicaid Services. (n.d.). Top 200 Level I HCPCS/CPT codes CY 2011. Retrieved January 22, 2014, from http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MedicareFeeforSvcPartsAB/downloads/LEVEL1SERV11.pdf?agree=yes&next=Accept
Centers for Medicare and Medicaid Services. (2012). Place of service code set. Retrieved January 22, 2014, from http://www.cms.gov/Medicare/Coding/place-of-service-codes/Place_of_Service_Code_Set.html
Centers for Medicare and Medicaid Services. (2014b, February 7). Claims processing manual. Publication 100-4. Chapter 25, section 75.1.
Centers for Medicare and Medicaid Services. (2014a). Healthcare Common Procedure Coding System. Retrieved January 21, 2014, from http://www.cms.gov/Medicare/Coding/HCPCSReleaseCodeSets/Alpha-Numeric-HCPCS.html
Centers for Medicare and Medicaid Services. (2014c). ICD-10-PCS official guidelines for coding and reporting. Retrieved January 22, 2014, from http://www.cms.gov/Medicare/Coding/ICD10/Downloads/PCS-2014-guidelines.pdf
Dougherty, M., Seabold, S., & White, S. E. (2013, July). Study reveals hard facts on CAC. Journal of AHIMA, 84(7), 54–56.
Fact sheets on CPT modifiers. (n.d.). Wisconsin Physician Services website. Retrieved January 22, 2014, from http://wpsmedicare.com/j5macpartb/resources/modifiers/
Federal Register. (1985, July 31). 50(147), 31038–31040.
Gill, C. J., & Gill, G. C. (2005). Nightingale in Scutari: Her legacy reexamined. Clinical Infectious Diseases, 40(12), 1799–1805.
Harris T. (1997, April 16). Physician’s Current Procedural Terminology (CPT). Statement of the American Medical Association to the Subcommittee on Health Data Needs, Standards and Security, National Committee on Vital Health Statistics Department of Health and Human Services. Retrieved January 21, 2014, from http://www.aapsonline.org/medicare/amacpt.htm
HIPAA Administrative Simplification: Modifications to medical data code set standards to adopt ICD-10-CM and ICD-10-PCS. (2009, January 1). Federal Register, 74(11), 3328.
King, M. S., Lipsky, M. S., & Sharp, L. (2002). Expert agreement in Current Procedural Terminology evaluation and management coding. Archives of Internal Medicine, 162(3), 316–320.
King, M. S., Sharp, L., & Lipsky, M. S. (2001). Accuracy of CPT evaluation and management coding by family physicians. Journal American Board of Family Practice, 14(3), 184–192.
Lott, T. (2001, July 27). Letter from Senator Trent Lott (R-Miss.) to Health and Human Services Secretary Tommy G. Thompson. Retrieved January 13, 2014, from http://www.aapsonline.org/medicare/lottcptletter.htm
Nirschl, R. (2001). Return to CPT 1991 E&M billing system. Bulletin of the American Academy of Orthopaedic Surgeons. Retrieved January 22, 2014, from http://www2.aaos.org/bulletin/feb01/ptvw.htm
Rousse, J. T. (2013, Summer). From novice to expert: Problem solving in ICD-10-PCS procedural coding. Perspectives in Health Information Management. Retrieved January 22, 2014, from http://perspectives.ahima.org/from-novice-to-expert-problem-solving-in-icd-10-pcs-procedural-coding/#.Ut_zSc7na70
Small, H. (1998). Florence Nightingale, avenging angel. New York, NY: St. Martin’s Press.
United States Public Health Service. (1959). International Classification of Diseases, adapted for indexing hospital records by diseases and operations. Publication No. 719. Washington, DC, U.S. Dept. of Health, Education, and Welfare, Public Health Service, National Center for Health Statistics.
U.S. Department of Health, Education, and Welfare, Public Health Service, Health Resources Administration, National Center for Health Statistics. (1975). Health United States 1975. DHEW Publication No. (HRA) 76–1232. Retrieved January 21, 2014, from http://www.cdc.gov/nchs/hus/previous.htm#editions
U.S. Department of Health and Human Services, Health Care Financing Administration, American Medical Association. (1998, July 28). Agreement. Retrieved January 21, 2014, from http://www.aapsonline.org/ama-hcfa-cpt-signed-agreement-1983.pdf
White, K. (n.d.). Reflections on the past and challenges for the future. The U.S. National Committee on Vital and Health Statistics. Retrieved January 21, 2014, from http://www.ncvhs.hhs.gov/ncvhs50white.htm

