14. Interdisciplinarity, Innovation, and Transforming Healthcare

James E. Stahl, M.D., C.M., M.P.H., is a practicing board-certified internist at Massachusetts General Hospital, Senior scientist at the MGH-Institute for Technology Assessment, Research Director for the MGH Outpatient RFID project, and Adjunct Professor in Mechanical and Industrial Engineering at Northeastern University. He is an outcomes researcher with expertise in decision science, health technology assessment, and simulation modeling. His current research focuses on clinical process redesign, the application of new technologies in the clinical environment, technology implementation, interdisciplinary collaboration, and ethics.
What Challenges Are We Trying to Solve?
Healthcare faces many challenges. The delivery of healthcare has become increasingly complex as medical science and technology advance at an ever-increasing pace. The system is fractured among multiple competing providers and stakeholders whose incentives don’t always align for the greater social good. Our mixed market economy has been relatively indifferent to quality and productivity in healthcare (Medicare 2006). Our population is aging and with age comes an increasing number of people with comorbidities and health problems. With increasing system complexity, system safety errors are rising. Recent reports indicate more than 100,000 drug-related, infection-related, or procedural errors in our hospitals (Care 2003; Century 2001; Series 2006; System 1999). This is why the Institute of Medicine (IOM) and National Academy of Engineering (NAE) have made a national call to arms to work for a healthcare system that is safe, effective, patient-centered, efficient, and equitable (Wilson and Howcroft 2005).
If these problems were simple, they would have been solved long ago. A common error when attempting to solve complex problems is to approach them from a single domain or perspective. We assume that the most salient feature of the problem is the cause, and if only we had a better scanner, antibiotic, procedure, or policy, the problem would go away.
Many problems in healthcare are complex and resist solutions via traditional single-domain approaches and are better addressed using an interdisciplinary, system-level perspective. There has been a growing recognition outside of healthcare that many major advances in science emerge out of interdisciplinary approaches (Klein 2000), and it is time this was applied more in healthcare.
However, there are also reasons why interdisciplinarity has not been widespread in healthcare. Simply, it is hard to do. Although interdisciplinarity offers opportunities for new insights and solving previous intractable problems (for example, hand hygiene), it also challenges comfortable work patterns and patterns of thought, as well as the organizational status quo.
What Is Interdisciplinarity?
Interdisciplinarity or transdisciplinary is a term increasingly used in health services but its definition is often unclear. In healthcare, interdisciplinarity can mean different things to different people and is often confused with multidisciplinarity. In clinical care, multidisciplinary teams can provide comprehensive care to patients. In this case multidisicplinarity might involve having providers from different clinical disciplines—for example, medical doctor (MD), registered nurse (RN), occupational therapist (OT), physical therapist (PT), social worker (SW)—working alongside each other (Zwarenstein, Goldman, and Reeves 2009). A care coordination team or a medical home might be examples of this.
Interdisciplinarity means something more. Interdisciplinarity is problem-solving perspective that integrates the knowledge and insights from many disciplines working together to achieve creative solutions (Armstrong 2006; Choi and Pak 2006; Fairbairn and Fulton 2000). To paraphrase Choi and Pak’s (Choi and Pak 2006) metaphor, multidisicplinarity is additive (for example, 2 + 5 =7), in which different types of knowledge are mixed together side by side but essentially remain distinct, whereas interdisciplinarity can be thought of as multiplicative or more (for example, 2 × 5 = 10). In interdisciplinary collaborations not only do team members come from disparate fields but the whole of the endeavor becomes more than the sum of its parts. The knowledge developed transcends the boundaries between disciplines, producing new forms of knowledge (Moran 2010).
As shown in many of the preceding chapters, effective interdisciplinary collaboration requires more than simply putting people from different disciplines in the same room together and hoping for the best (Klein 2000). In many ways, interdisciplinary collaboration is a paradigm for all collaboration, ”a process through which parties who see different aspects of a problem can constructively explore their differences and search for solutions that go beyond their own limited vision of what is possible” (Gray 1989). To be effective, not only do different knowledge domains need to be bridged but also worldviews (Porter and Rossini 1984). Philadelphia University recognized this in the creation of their integrated college (DEC) and therefore crafted a core curriculum to establish common tools and language across the integrating disciplines. These tools were designed to facilitate collaboration and enable interdisciplinarity, as opposed to melding disciplines into a single viewpoint or simply coordinating a more streamlined multidisciplinary approach.
In healthcare, many differences in perspective can be traced to the distinct discipline (Leipzig 2002), which can root them in different problem-solving approaches (Choi and Pak 2006, 2007), or a person’s role in the healthcare system (Glouberman and Mintzberg 2001a, 2001b), which gives them different stakes in the outcomes.
Facilitating Interdisciplinarity
In 2011, we conducted a workshop (Radcliffe Center) on facilitating (Witteman and Stahl 2013). The key tools were drawn from a wide variety of disciplines and were focused on facilitating interaction and communication among a diverse group (clinicians, industrial engineers, economists, industrial designers, human factors engineers, social scientists, entrepreneurs, nurses, psychologists, and others) to solve “wicked problems” in healthcare. “Wicked problems” are problems that are notably intractable due to their being subject to multiple competing and cross-influencing inputs and feedback mechanisms. In fact, the teams were not only tasked to map and solve the solution space around a wicked problem but also map and define the problems themselves. The problems identified and tackled in this workshop were patient-clinician communication and hand hygiene.
These were the key elements:
• Frameworks and tools: It is important to set up an explicitly interdisciplinary framework and tools for problem solving and problematizing.
• Deep dives: This is a technique popularized by IDEO, an industrial design firm. Deep dives are a form of immersive facilitated brainstorming usually targeted at specific end-user needs, often making use of tools and frameworks.
• Improvisational games: We used improvisational games, specifically, along the lines of the work of Viola Spolin. These improvisational games are about unearthing creative responses in the context of tight constraints and building team communication, for example, the “Yes, but...” game. Similar to the “Yes, and” improvisational game described in Chapter 9, “Navigating Spaces—Tools for Discovery,” which focuses on building, here every individual must start every interaction with “Yes, but....” This forces the person speaking to explicitly accept what the previous person said and then explicitly turn it into something else.
• Rapid visualization: We had a team of industrial design students attend whose sole job was to rapidly draw and visually articulate on walls covered with paper for this purpose, ideas verbalized by the teams. This created an external object/representation, which all team members could respond to, add to, or edit. This helps answer the question “Do you see what I see?” and helps bridge interdisciplinary gaps in language (Lattuca 2001).
Even the best techniques and tools can only go so far. Other key considerations in successful interdisciplinary collaborations to consider are personality types as described in Chapter 5, “The Role of Learning Styles in Innovation Team Design,” and communication styles and problem-solving styles as described in Chapter 6, “Your Team Dynamics and the Dynamics of Your Team.” Solving complex problems by adopting interdisciplinary, systems-level perspectives often requires challenging the usual ways of approaching problems. Significant previous work on problem-structuring methods has shown the potential of interdisciplinary approaches, but has noted the difficulty of orienting people to new ways of tackling long-standing challenges (Mingers and Rosenhead 2004). This kind of shift in attitudes and methods can be difficult in any context, and healthcare presents particular challenges related to disciplinary roles at the professional, administrative, and academic levels (Glouberman and Mintzberg 2001a, 2001b). Participants in these exercises must be willing, engaged, and to some degree open to new ideas and approaches if the process is to succeed, hence establishing an explicit interdisciplinary framework before starting.
We suggest that setting teams off on the right track and giving them the tools they need to adapt to change might help, and the concepts and tools explored in our workshop do precisely that. These four techniques are designed to be used at the beginning and formative part of a project and also intermittently through the project to catalyze breakthroughs, get out of dead ends, or take a project in new directions as more is learned, which is inevitable with complex problems.
Innovation, Technology Adoption, and Change in Healthcare
One way to define technology is that it is any instrumentality that facilitates the end-users’ ability to achieve their goals. By this definition, technology can be a device, a test, or even a policy or process. Innovation is another word that means different things to different people. Traditionally, innovation implies a new or different solution to a problem or set of needs, a new technology that meets the new or changing goals of the end users. Recently, though, the word has often been conflated with process improvement, which is doing the same task more efficiently.
A new technology thus falls into one of two broad categories: efficiency solutions and transformative solutions, or as described in Chapter 3, “Framing the Vision for Engagement,” optimization innovation versus development or formulation innovation. An example of an efficiency solution is a new CT scanner that is 10% faster than its predecessor, which is aimed to help problems with episodes of high patient volume. The salient problem is time in the CT scanner, which the problem addresses through optimization. The deeper problem is why the CT scanner was having episodes of congestion in the first place. An example of a transformative solution is the use of real-time locations systems to get the patients to the right place at the right time with the right resources, such as the CT scanner. This is an example of more upstream innovation in the realm of discovery and formulation in the opportunity recognition phase. Here the solution changes how work is done by enabling end users to visualize, contact, and coordinate current resources to get more out of the same resources. It is also a new technology that at relatively little expense measures things we have not been able to measure before.
However, either type of solution is meaningless unless it is adopted, and technology adoption is usually an interdisciplinary problem. At the macro level every change in healthcare must satisfy the competing and cooperating groups that represent cure (MDs), care (RNs), control (managers), and community (trustees) (Glouberman and Mintzberg 2001a, 2001b). At the micro level no technology succeeds unless supported by the end users and intermediate managers. There is a wide literature on technology adoption and implementation science. For technology to be accepted, it must satisfy perceived usefulness, perceived ease-of-use, social norms, and many other constraints imposed by competing groups. In our own work of rolling out a clinical RTLS, we found “trust” in how the technology is to be used and “trust” in the person promoting or supplying it is essential.
Trust is gained in several ways. One important way in healthcare is through evidence. Based in both science and art, healthcare responds to outcomes or activities that can be validated. However, the evidentiary demands vary from stakeholder to stakeholder. For example, a clinician may only accept evidence based on large experimental trials and will seek to optimize practice and wait for the evidence to come in before changing, whereas healthcare managers may choose to “satisfice,” that is, make the best available choice with the information they have at the time the decision needs to be made for other reasons. The world of evidence medicine is too large to summarize here; however, suffice it to say that there are varying accepted degrees of evidence based on their source and reliability.
Two useful sources of evidence in interdisciplinary collaboration and innovation in healthcare are simulation and rapid prototyping. Simulation is the study of systems or technologies in which the system being studied reproduces the same cause-and-effect relationships found in the real-world example. Simulations can be in silico, that is, computer programs, or physical like simulation labs where clinical procedures are performed on mocked-up patients. Through experimentation such as sensitivity analysis and “what if” scenario experiments, the performance characteristics and boundaries of performance can then be explored. As discussed extensively in previous chapters, notably Chapters 9 and 10, rapid prototyping is the process building of physical prototypes that reproduce the solution being articulated, which then in turn receives immediate feedback on its success or failure by stakeholders. It is then iterated rapidly and repeatedly until a solution acceptable to the end users is identified.
We have used both methods extensively in a variety of projects.
The OR of the Future Project (ORF)
The ORF was aimed to address the problem of surgical demand. Demand for surgical services continues to rise faster than our ability to supply them (Hall and DeFrances 2003). In an increasingly resource-constrained environment, efficiency is critical for maintaining access to quality care. At the same time, we must maintain quality and safety without burning out our clinicians who supply these services.
Surgeons, nurses, and OR administrators often turn to new technologies to help solve this problem. However, in the OR setting, new technologies are usually introduced in an ad hoc manner without rigorous analysis of their potential costs and benefits. Our hypothesis was that by bringing an interdisciplinary team together, we could reinvent the OR both physically and organizationally to solve the OR-level constraints on surgical demand.
We designed the ORF to be a living laboratory where we could measure the effect of new staffing regimes, peri-operative systems (in-hospital systems surrounding and supporting surgical process), and equipment on the delivery of surgical care. This project was a collaboration among multiple stakeholders—Massachusetts General Hospital (MGH); Center for Integrated Medicine and Technology (CIMIT); a consortium of physicians, scientists, and engineers from the Harvard University Medical School teaching hospitals; Massachusetts Institute of Technology (MIT); and Charles Stark Draper Laboratory. The project team included surgeons, anesthesiologists, nurses, operating room (OR) administration, patients, bioengineering, operations researchers, and health outcomes researchers. The ORF team conducted a landscape survey of surgical state-of-the-art ORs in both the United States and Europe, searching for examples of best practices in OR and perioperative system design.
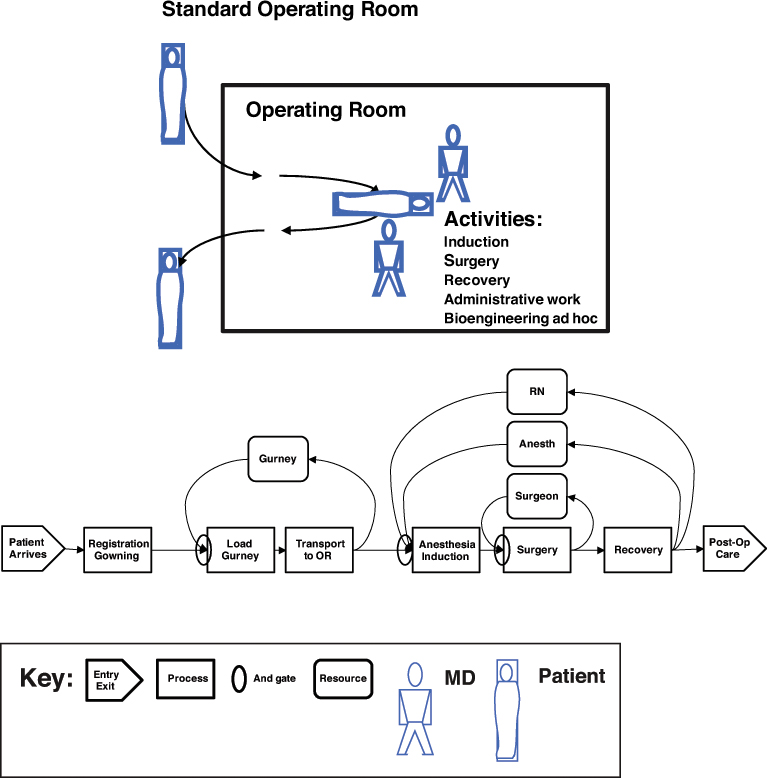
The main distinguishing feature of the ORF design was a central operating room with attached induction and recovery bays and a control room to provide a workspace for surgeons between cases. The operating room itself was equipped with an integrated OR system, mobile booms (suspending equipment from the ceiling, freeing floor space and allowing for flexible equipment configurations), and combined gurney/table systems. The redesigned perioperative process enables staff to care for patients in parallel or in an interleaved fashion, in contrast to the traditional sequential process, enabling up to three patients to be cared for simultaneously in the induction bay, the OR, and the recovery bay. However, this process change requires more staff (an additional 0.5 anesthesia FTE [full-time equivalent] and 1 nurse FTE) than in the standard OR process (Stahl et al. 2005; Stahl, Goldman, Rattner, and Gazelle 2007; Stahl et al. 2004; Stahl et al. 2006).
Before proceeding, however, decision makers in the hospital had to be convinced that it was worth the effort, that is, taking two operating rooms offline while constructing the new ORF, and had to be convinced that the new system would be worth the added expense after it was running.
Physical mock-ups were made to work out potential new clinical workflows, and the knowledge from these exercises and from the landscape survey were instantiated in a computer simulation model. This model was then used to adjust the physical design and test the boundaries of its behavior with regard to quality, safety, and cost (Stahl et al. 2004). These analyses were then used as evidence to build trust and help convince decision makers to build the ORF.
This process was taken full circle in that after the ORF was built and in operation, the initial model predictions were put to the test, and the computer simulation predictions did indeed predict future performance accurately.
This exercise in evidence-based design informed subsequent OR design in our hospital and other hospitals (see Figures 14.1a and 14.1b).
Evidence-based design is a developing field used by architects, industrial designers, and project planners in which designs are vetted based on the new structure’s health outcomes, economic performance, productivity, customer satisfaction, and other measures. Specifically, in the context of healthcare, it explores what elements or systems of elements promote the organizational mission (usually, healthcare access, quality, and safety) of the healthcare facility. Lessons learned from these trials presumably can be transferred to other projects.
Interdisciplinarity enabled the team to explore the problem space and vet the solutions, generate ownership among a broad coalition of stakeholders and evidence for decision makers, and create something new in the difficult healthcare environment.
Aha! Moments
Reflecting on our efforts from the operating room of the future, we uncovered a series of key insights, notably the following:
• Language and culture matter.
Assembling this interdisciplinary team was necessary but not sufficient. Once together, they had to be able to work together. Immediately, language became an issue. Each group had its own culture, its own language and way of approaching problems. Creating a unified language and goal was primarily achieved using a systems engineering perspective teaching the team as a whole how systems behave from their own individual piece to the integrated whole. With this came a new unifying language, which, in part because it was new to everyone, was acceptable by everyone.
• Personalities matter.
As you can imagine, in a mix of these types of disciplines there were many strong personalities and several blocking personalities. Here, leadership and negotiating skills and understanding the nature of the competing-cooperating healthcare environment is essential.
• Ownership matters.
In complex organizational environments ownership can be ambiguous, and when ambiguous often fraught with anxiety. Allowing people to take ownership gives them motivation to see the project succeed. The key solution in this case was to take a lesson from Harry Truman, who said, “It is amazing what you can accomplish if you do not care who gets the credit.” This is often difficult in an academic setting; however, credit does seek its proper attribution with time.
• Computer simulation does predict reality.
Simulation is a key method for bringing stakeholders together, improving design, identifying bugs before they happen, predicting future behavior, and generating evidence for decision makers (Stahl 2008).
Hand-Hygiene and Healthcare-Acquired Infections
This methodology has wide application. We are currently applying it to the hand-hygiene problem. Hand hygiene is a classic wicked problem, and has been for at least 150 years, since Ignaz Semmelweiss first identified it in Austria in the 1850s. There are likely more than 100,000 preventable hospital-acquired infections each year in this country, the majority of which could probably be eliminated if there was an effective, consistent way of decontaminating clinicians’, and patients’, hands between patient-clinician interactions.
The hand-hygiene problem has for the past 150 years been approached from the traditional single-domain perspective, repeatedly. Our soaps remove but don’t kill the infectious agents; therefore, let’s develop bactericidal soaps. It takes too long to clean our hands; therefore, let’s develop desiccating agents such as alcohol-based gels. People don’t know how to wash their hands properly or forget; therefore, we institute an education campaign; and so on. Yet hospital-acquired infection rates remain relatively static.
Our hypothesis was that any problem so resistant to change must be multidimensional and be a complex system of positive and negative feedback. To that end, we gathered an interdisciplinary team of infectious disease specialists, clinicians, industrial engineers, industrial designers, architects, behavioral and cognitive psychologists, patients, and others. The team was set the task of defining the problem space and mapping out the solution space with the specific goal of identifying the characteristics of key solutions.
Any complex system tends to be resilient. In the case of hand hygiene, the system is resilient at an undesirable system state. The key, then, is to find an achievable method to shift the state of the system.
Hand-hygiene activity is dependent on the workflow and physical space: Are there opportunities to clean your hands—for example, sinks available when you need them? It is dependent on perceptual, cognitive, and behavioral psychology factors. If I cannot see the dirt, I won’t be prompted to wash it off. If my brain is occupied by too many other tasks, the hand-hygiene task gets bumped off the list. If my peers don’t wash regularly, why should I? And so on. It is dependent on knowledge and skill: Do I know the circumstance in which to clean my hands and with what, soap or gel? Is it okay to wash my hands 30 seconds, 1 minute, half an hour before seeing the patient? And so on, to name a few of the complexities surrounding this behavior.
A key element to solving this problem is appropriate feedback based on reliable, trustworthy measurement. Our current state of the art is inadequate. The current gold standard, that is, having designated observers sampling behavior in clinical units, suffers from small sample size and the risk of modifying the behavior that the observers have been tasked to observe. Sending in “secret shoppers” suffers even worse sample-size considerations and often has even more limitations on the activities observed. Measuring the quantities of soap or gel used is rough at best. Results from these tools are fed back to the end users at often substantially delayed intervals (for example, monthly or quarterly) and often in aggregate. As a result, end-user behavior is challenged only intermittently and enough time has passed that the link between cause and effect has been attenuated and people don’t know how relevant the feedback is to them.
One potential solution identified was to marry hand-hygiene measurement with real-time location systems to provide feedback at the time and place the patient-clinician activity is taking place. To this end, we developed a prototype system in which a signal is fed back to the clinician when the patient and the clinician are in the exam room together and an appropriate interval has passed.
We also developed a simulation model of the work flow and physical landscape in which this activity occurs, which we are using to explore issues of cost, benefit, and adherence. Results from this project should be published in 2014.
Discussion
The important challenges in healthcare are increasingly “wicked problems.” New technologies and social trends such as point-of-care testing, ubiquitous sensing environments, the challenge of aging in place, new payment systems, and others offer new challenges that might transform what it means to deliver healthcare. If we are to bend the cost curve and maintain quality and safety, we can no longer constrain ourselves to in-the-box thinking. In fact, we need to reach across disciplines, across industries and modes of thought, to identify solutions. True interdisciplinarity offers a way to promote creativity and manage change. We need to have the courage to embrace change before we are forced to change.
Take-Away Points
From our experiences piloting learning launches of interdisciplinarity in healthcare, we note a set of key takeaway points, specifically the following:
• Interdisciplinarity offers a way of solving problems previously thought intractable.
• Avoid narrow teams.
Avoid the trap of single-domain teams or even multidisciplinary teams, and include people who are stakeholders but might not normally interact and, if possible, people who are not stakeholders.
The broader the range of perspectives, the more likely you’ll truly understand the problem space.
The broader the range of solution styles, the more likely you’ll find a solution that is workable and sustainable.
• Putting teams together is not enough; they need the right tools to work successfully.
• Provide a safe environment with the space and time to experiment.
• Prototype solutions and use these prototypes to simulate the new experience if you want robust workable solutions.
• Be prepared to listen and have courage and perseverance.
Interdisciplinary problem solving tends to be disruptive, and both exploring and solving a wicked problem will likely require challenging and changing the factors that make the problem resilient. These factors often include culture, political, and organizational structure.
References
Armstrong, P. 2006. Advancing Interdisciplinary Health Research: A Synergism Not to Be Denied. Canadian Medical Association Journal, 175(7), 761–762.
Care, P. S. A. a. N. S. f. (Ed.). 2003. Washington, DC.
Century, C. t. Q. C. A. N. H. S. f. t. s. (Ed.). 2001. Washington, DC.
Choi, B., and A. Pak. 2006. Multidisciplinarity, Interdisciplinarity and Transdisciplinarity in Health Research, Services, Education and Policy: 1. Definitions, Objectives, and Evidence of Effectiveness. Clinical and Investigative Medicine, 29(6), 351–364.
Choi, B., and A. Pak. 2007. Multidisciplinarity, Interdisciplinarity, and Transdisciplinarity in Health Research, Services, Education and Policy: 2. Promotors, Barriers, and Strategies of Enhancement. Clinical and Investigative Medicine, 30(6), 224–232.
Fairbairn, B., and M. Fulton. 2000. Interdisciplinarity and the Transformation of the University. Saskatchewan, Saskatoon: Centre for the Study of Co-operatives. University of Saskatchewan.
Glouberman, S., and H. Mintzberg. 2001a. Managing the Care of Health and the Cure of Disease—Part I: Differentiation. Health Care Management Review, 26(1), 56–69.
Glouberman, S., and H. Mintzberg. 2001b. Managing the Care of Health and the Cure of Disease—Part II: Integration. Health Care Management Review, 26(1), 70–84.
Gray, B. 1989. Collaborating: Finding Common Ground for Multiparty Problems. San Francisco: Jossey-Bass.
Hall, M., and C. DeFrances. 2003. National Hospital Discharge Survey. Advance Data Vital and Health Statistics, 332.
Klein, J. 2000. A Conceptual Vocabulary of Interdisciplinary Science. In Practicing Interdisciplinarity. Toronto: University of Toronto Press.
Lattuca, L. 2001. Creating Interdisciplinarity: Interdisciplinary Research and Teaching among College and University Faculty. Nashville, Tennessee: Vanderbilt University Press.
Leipzig, R. 2002. Attitudes Toward Working on Interdisciplinary Healthcare Teams: A Comparison by Discipline. Journal of the American Geriatrics Society, 50(6), 1141–1148.
Medicare, R. P. P. A. I. i. (Ed.). 2006. Washington, DC.
Mingers, J., and J. Rosenhead. 2004. Problem Structuring Methods in Action. European Journal of Operational Research, 152(3), 530–554.
Moran, J. 2010. Interdisciplinarity: The New Critical Idiom. London: Routledge.
Porter, A., and F. Rossini. 1984. Interdisciplinary Research Redefined: Multi-Skill, Problem-Focussed Research in the STRAP Framework. R&D Management, 14(2), 105–111.
Series, P. M. E. Q. C. (Ed.). 2006. Washington, DC.
Stahl, J. 2008. Modelling Methods for Pharmacoeconomics and Health Technology Assessment: An Overview and Guide. Pharmacoeconomics, 26(2), 131–148.
Stahl, J., M. Egan, J. Goldman, D. Tenney, R. Wiklund, W. Sandberg...D. Rattner. 2005. Introducing New Technology into the Operating Room: Measuring the Impact on Job Performance and Satisfaction. Surgery, 137(5), 518–526.
Stahl, J., J. Goldman, D. Rattner, and G. Gazelle. 2007. Adapting to a New System of Surgical Technologies and Perioperative Processes among Clinicians. J Surg Res, 139(1), 61–67.
Stahl, J., D. Rattner, R. Wiklund, J. Lester, M. Beinfeld, and G. Gazelle. 2004. Reorganizing the System of Care Surrounding Laparoscopic Surgery: A Cost-effectiveness Analysis Using Discrete-Event Simulation. Medical Decision Making, 24(5), 461–471.
Stahl, J., W. Sandberg, B. Daily, R. Wiklund, M. Egan, J. Goldman...D. Rattner. 2006. Reorganizing Patient Care and Workflow in the Operating Room: A Cost-effectiveness Study. Surgery, 139(6), 717–728.
System, T. E. i. H. B. A. S. H. (Ed.). 1999. Washington, DC.
Wilson, M., and D. Howcroft. 2005. Power, Politics and Persuasion in IS Evaluation: A Focus on Relevant Social Groups. Journal of Strategic Information Systems, 14(1), 17–43.
Witteman, H., and J. Stahl. 2013. Facilitating Interdisciplinary Collaboration to Tackle Complex Problems in Health Care: Report from an Exploratory Workshop. Health Systems, 1–9.
Zwarenstein, M., J. Goldman, and S. Reeves. 2009. Interprofessional Collaboration: Effects of Practice-Based Interventions on Professional Practice and Healthcare Outcomes. Cochrane Database of Systematic Reviews Online 3(3), CD000072. doi:000010.001002/14651858.CD14000072.pub14651852.