7. Tough It Out versus Stay at Home: Modeling Disease Spread Through Face-to-Face Conversations
When you get sick, do you go to work?
Although on its face this is a simple question, it has a far from simple answer. What humans are instinctually driven to do isn’t necessarily a product of an evolutionary response to disease, nor is it based solely on our upbringing. The culture of our company and country can play a huge role.
From a physical health perspective, obviously staying home is better. There are no debates. If you stay at home when you’re sick, you are unable to infect anyone else. Many public health professionals would argue that by staying home you’re making a positive decision for society. Fewer people get sick, fewer people miss work, and all it costs you is one day of productivity.
However, the actual cost might be far higher. From a productivity perspective, whether you go to work has a huge impact not just on yourself, but on your coworkers. As discussed in Chapter 4, when you don’t interact with people that you work with, everyone’s performance suffers. A lack of communication also negatively impacts job satisfaction levels, and consequently, mental health outcomes.
Companies continually grapple with this quandary, as the following personal experience illustrates. A few years ago I took time off from my graduate studies at MIT to work as a researcher for a large Japanese electronics company in a lab near Tokyo. I had collaborated with some researchers from this lab, and in order for us to work together at a more meaningful level, I had to be an employee. As an undergraduate, I had minored in Japanese, so I was also thrilled at the opportunity to return to Japan and shore up my language skills. I had worked in other labs in Japan before, and because I could speak the language, I felt like I was prepared for the cultural differences that awaited me there.
Japanese offices, and Japanese research labs in particular, are very different from those we have in the U.S. A typical lab has an extremely large bullpen area, with hundreds or even thousands of researchers sitting across straight rows of open desks. Desks might have a small cubicle wall, but if you stand up, you can easily see everyone in the lab.
Face time is also highly valued. Researchers arrive fairly early, around 8 a.m., but normally won’t leave until around 8 p.m. Everyone eats lunch and dinner together in the cafeterias. The environment is designed to foster interaction and keep people at work for as long as possible.
One day during my time at this Japanese research lab, I got sick. Not the kind of sick where you have a light headache that you can quickly kill off with some aspirin, but the 101-degree fever sit in your bed wearing an oversize sweatshirt while watching Law and Order reruns kind of sick. My conundrum was that my team had a presentation coming up the next day, so I had to finish up the materials we needed to show our manager.
After seeing that I was looking pale and generally out of sorts, one of my colleagues came over to my desk to see what was the matter.
“I’m coming down with something,” I told him honestly. “I’ve got to stay here and finish the slide deck, but I probably won’t be able to make the presentation tomorrow.” He looked at me very seriously.
“No, you have to go home right now,” he replied. I was a bit confused, and I thought that maybe I had made a mistake in my Japanese. You weren’t allowed to bring company computers home with you or e-mail attachments outside the company, so finishing up at home was out of the question.
“I really need to finish this by tomorrow, so I have to stay and finish it today,” I reiterated. He shook his head.
“No, you really have to go home right now,” and with that I was politely excused from the lab. In a mild state of shock, I took the train back to my apartment and considered how I should respond. I knew that I had to finish this presentation, so I figured the best course of action would be to arrive at the lab early the next day and leave myself enough time to complete everything.
When I arrived, I was politely told that I had to wait at least one day before coming back. They just wouldn’t let me back into the lab under any circumstances until they were convinced I was healthy. In Japanese companies, the desire for face time and even productivity is vastly outweighed by a mysophobia (fear of germs) that borders on the extreme.
For those of us from the U.S, this hard-line reaction to illness seems strange. Imagine telling your boss: “Hey, I know we’ve got an important deadline tomorrow, but I’m feeling under the weather, so I won’t be able to make it.” You would at least expect a bemused reproach, if not a downright reprimand.
United States workers doggedly insist on meeting professional obligations even if they have personal issues that could conflict with these obligations. When a child is born, parents aren’t guaranteed pay for the time they take off, and after 12 weeks, their employer could legally fire them if they haven’t returned to work. So it’s no surprise that when we come down with an illness, employers are less than forgiving.
In a different personal example, I was on a business trip where I had to work while running a fever of 102 degrees for three days. Somehow I managed to be halfway productive, but for the week after I returned home, I was in a constantly weakened state, not to mention the fact that I probably infected a number of my colleagues. This would cause a ripple effect in terms of lost productivity. Instead of only one person out of commission for a few days, all of a sudden you have a dozen people working at vastly reduced effectiveness and feeling miserable in general.
It’s easy to understand why companies cultivate a “tough it out” ethos. Unless you can work from home, your productivity when you’re out sick is zero. As shown in all the studies mentioned in this book, even working from home isn’t very effective because face-to-face communication with your coworkers dramatically improves your performance as well as that of all the people with whom you normally interact. If you stay at work, even though your effectiveness will be reduced, you can still take advantage of all the social productivity effects that the studies in this book uncovered.
So, which response is correct?
To answer that question, real-world behavioral data is needed to understand how diseases spread within companies, using methodologies developed by epidemiologists. This allows us to estimate how changes in behavior from disease responses impact productivity. Using data from the IT firm introduced in Chapter 5, that’s exactly what we did.
Corporate Epidemiology1
The IT firm project is a great dataset for investigating the effectiveness of disease response strategies. Recall that in this study dozens of people configuring complex hardware systems wore Sociometric Badges for about a month. Besides the badge data, we also had hard productivity numbers, allowing us to create a very accurate model of performance based on behavior.
When people get sick, their behavior changes. To see what sort of effect this would have, we can modify the behavioral patterns extracted from the original IT firm data and observe how productivity would change. Specifically, we look at how the cohesion changes for each member of the firm, because that was the feature most strongly correlated with performance.
In this exercise we simulate people getting sick in the original dataset, simulate the infection spreading, and calculate the effect this illness has on performance. The goal is to see what happens if people change their behavior when an outbreak occurs. For example, if people go straight home when they become sick, we can remove their interactions from the original dataset for the days when they are “at home.” This changes the interaction patterns in the entire group, and using our performance model, we can see how this behavior change affects the bottom line.
To simulate the spread of the disease, fellow MIT researchers Manuel Cebrian, Riley Crane, and I collaborated with epidemiologists Leon Danon and Ellen Pollock from Harvard’s School of Public Health. One major aspect of this model was determining how to simulate disease transmission and recovery. Luckily, the public health field has studied these processes extensively. Transmission probabilities are derived from transmission methods and virus lifecycle estimates in the academic literature (the now-famous R0 value popularized in the movie Contagion). Recovery times are also relatively easy to estimate. Researchers will observe infected individuals in controlled environments, typically a laboratory, and take blood samples over the course of a few days to see how long someone takes to recover.
We used a standard infectious disease simulation method called an SIR (Susceptible-Infected-Recovery) model. Each stage of the SIR model has different properties, and at any point in time any individual is in the S, I, or R stage. In the S stage you’re not sick, but you might become infected (although for certain types of disease, not everyone is susceptible). After you’re infected, you enter the I stage. At this point you can infect other people for a set period of time. Each time you interact with a person in the S stage, the simulation program picks a random number to determine whether that person becomes infected. In reality even after you contract the disease, you are not immediately infectious because the disease needs time to spread through your body. However, this doesn’t make a big difference in the outcome of any simulation because for most illnesses becoming infectious takes only an hour or two.
After a few days, you enter the Recover stage. In this stage you can’t infect other people or be infected, and this is the virtual analogue of the immunity you acquire after having been exposed to an illness. Many of us have experienced this in our own lives. After you have a fever, it’s not uncommon that one of your family members will get sick as well. Even though other family members might catch the bug too, you stay healthy because your immune system has learned to fight off the disease.
In terms of hard numbers, interacting with an infected individual for one minute in our model gives you a 0.7% chance of infection. Full recovery after infection, on the other hand, takes three days. These numbers are roughly equivalent to the epidemiological characteristics of H1N1.
Now that we have the data and the model, how do we start things off? In other words, how do we choose who gets sick first so that we can see how the disease will spread? The answer is that we don’t. For every individual in the data, in the beginning of every day for a one-week period, we start a simulation with that person labeled “infected.” This creates different paths of infection through the workplace, because we don’t really know who is more likely to get sick beforehand. Each of these infection starting points is simulated a few hundred times. The reasoning behind this method is that depending on how lucky you are, different people will get randomly infected when simulating this epidemic. Even with real data, there is a chance that many more people will get randomly infected in a single simulation simply because the random number generator happened to pull the right numbers out of a hat. We need to average over these different simulations to ensure an accurate picture emerges of what we would expect to happen. Adding in the extra wrinkle that different people are the starting points for infections provides a robust view into the dynamics of this disease.
During the initial simulations, we didn’t change behavior at all. We just wanted to see what the dynamics of the disease propagation looked like: Were certain individuals responsible for most of the disease spreading? Did certain types of interactions lead to the majority of infections?
What we observed was initially very puzzling. Although longer interactions did tend to lead to infections, the shorter interactions were responsible for the lion’s share of disease propagation. It makes sense that longer interactions would lead to infections. Mathematically, if an infected person talks to a healthy individual for more than 100 minutes, then a greater than 50% chance exists that the healthy person will become infected. Compare this probability to what happens if I talk to 20 people for 5 minutes each: The likelihood that I will infect a single person is the same—50%. The likelihood that I would infect a specific individual, on the other hand, is only 3.5%. However, if I infect one of the first people I talk to, then after our 5-minute conversation, we can both go on and infect other people. These dynamics are what caused most of the infections we observed.
As we were wrapping our heads around this concept, we wondered what would happen if we were able to reduce those interactions. Rather than completely cutting off all interaction as we initially proposed, we wanted to investigate the effect of removing only these very short conversations. We didn’t have a good idea of exactly what the cutoff should be, so we simply tried them all.
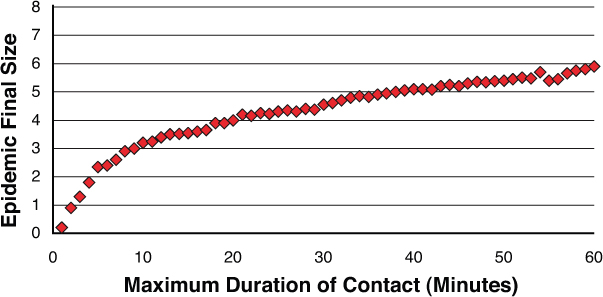
Figure 7.1 shows the number of people who got sick (the epidemic final size—vertical axis) as we put a higher and higher threshold on the minimum duration of a conversation (horizontal axis). So for the point of minimum contact duration of 5 minutes, we eliminated all interactions that lasted less than 5 minutes and repeated the simulation. As you can see, this 5-minute period seemed to be the perfect cutoff point, reducing the number of people who got sick by almost 50%. After this 5-minute period, only slight reductions occur in the epidemic’s size.
We also wanted to see what happened if we put a maximum threshold on interactions, eliminating only conversations that were longer than a certain amount of time. As you can see from Figure 7.2, we don’t observe a similar effect. To achieve a result equivalent to what we observed at 5 minutes in the graph shown in Figure 7.1, every interaction longer than 25 minutes would have to be eliminated.
Still, the question about the effect on productivity remains. What would this kind of behavior change (that is, removing conversations of a certain duration) do to the productivity of the division? In these same simulations we also computed how the networks of the division changed. By speaking a little bit less, or not at all, to other people in the division, performance was substantively affected.
Figure 7.3 shows the percentage change in the division’s overall performance that results from removing interactions falling below a duration threshold. The minimum duration of conversation numbers show a very interesting bump in productivity around the five-minute mark. According to the data, productivity would actually improve by eliminating these very short interactions.
Here is the disconnect between modeling and reality: Shorter interactions tend to be largely informal, such as bumping into someone you know in the hallway or chatting by the coffee machine. For people whom we are very close to, we’ll have deeper conversations in addition to these short ones. People with whom we only casually chat, however, probably don’t run in the same social circles, which is why removing those interactions would yield an increase in cohesion. This would imply that we should universally strive to eliminate these short conversations.
In the short term, there are certainly advantages to this practice. People would be able to spend more time talking to their close contacts, making it easier to communicate complex information and building trust. On the other hand, eliminating these interactions would slowly erode the connectivity of the overall division. After these weak connections are removed, the group would eventually become an echo chamber because group members would only be talking to each other. As we’ve already discussed, that would be a huge mistake.
Therefore, we should interpret these results more in the context of epidemic risk than as a general rule for how to shape communication patterns. The results clearly state that during high-risk periods, reducing the number of short interactions will greatly decrease the number of people who get sick and might even have some performance benefits. At the very least we wouldn’t expect productivity to suffer.
Eliminating longer interactions, however, is a different story. As Figure 7.4 shows, eliminating longer interactions has a consistently negative effect. This effect comes from the fact that you can spend long periods of time talking with the people with whom you work closely, and a reduction in those interactions will almost always decrease the cohesiveness of your network. For comparison, removing interactions longer than 30 minutes would result in a 1% decrease in productivity.
Now that we know what effect these different interventions have on health and productivity, the question becomes how to implement them. The focus shouldn’t just be on reducing the number of short conversations. Although this represented a nice tradeoff between health and performance, in some circumstances health concerns will preempt performance issues. In those cases reducing both shorter interactions and longer ones would be helpful in an effort to clamp down on the spread of a disease. This is when staying at home becomes an attractive option.
Many strategies are available for reducing the number of short conversations. As previously discussed in Chapter 4, distance has a powerful influence on interactions. The closer you sit to someone, the more likely you are to speak with that person. This is especially true for short interactions. If you’re going to spend an hour in a meeting with someone, the distance to his desk doesn’t matter. Walking over to him or finding a meeting room is worth your while. However, distance has a huge impact on serendipitous interactions. When your desk is physically closer to people you know, you’re more likely to bump into them or engage in some chit-chat.
We can use this tendency to our advantage by piggybacking on current trends in the workplace, namely the concept of open seating. In open seating offices, no one has an assigned desk. Instead, different groups sit in different areas, and people in a particular group can choose any desk in their area either for a single day or for at most a few weeks. Instead of keeping groups together, mixing up the different groups would increase the average distance between people on the same team. This would mean fewer serendipitous interactions because you would be farther away from the people you normally talk to.
This seating arrangement wouldn’t be the policy all the time, and would only apply during high-risk periods. At the beginning of an outbreak, companies could shift their work areas to “epidemic seating.” This costs the companies practically nothing, doesn’t inconvenience employees, and has a positive impact on health. You could also imagine some side benefits from this effort, because you might get to know people in other groups whom you don’t normally talk to. We might think this would defeat the purpose of the new seating arrangement, but these would actually tend to be longer interactions because you have to introduce yourself at length. In any case short interactions will occur more infrequently than they would in a normal seating arrangement.
Another simple strategy for reducing short conversations involves keeping office doors closed. An open door makes it easy for people to poke their head in and say hello, which under normal circumstances would be welcome. By keeping office doors closed, someone can still easily come by, but it would be a more intentional interaction, which would typically last for a longer period of time.
To make a major reduction in the number of short conversations, another effective strategy is to increase the number of long interactions. During high-risk periods, companies could schedule “Meeting Days” where every meeting for the next few weeks is crammed into a few days. This approach would create a large number of very long interactions, but would all but eliminate short conversations. If for various logistical reasons this is not possible to fully implement, even a partial shift of meetings to high-risk periods would have a marked effect.
Making small changes to reduce long interactions, on the other hand, is relatively hard. These interactions tend to be planned and more critical than short ones. Therefore, you have to change intention and formal processes more than changing the environment slightly to encourage certain behaviors. A simple step would be to eliminate meetings longer than a certain amount of time. You could also move meetings to video conference, but that would significantly degrade the quality of the meeting.
Given the impact on performance, however, reducing long interactions represents a fairly drastic step and would only be taken in extreme cases. In general, this means that the best way to eliminate long interactions is for people to stay at home. However, impacting the primary mechanism of airborne infections is also possible through cultural changes.
In Japan people wear surgical masks when they’re sick so that they pass fewer germs to others. Because the mask blunts the velocity of expelled air and most infections are caused from talking to other people, this intervention would actually be quite effective.
Table 7.1 summarizes different strategies that organizations can adopt to combat disease while balancing the impact on productivity. Depending on the situation, a company might want to place more emphasis on health, but in another situation context may become more important. The strategies presented here shouldn’t be viewed as a list of things that have to be implemented for every disease outbreak, but rather part of a toolbox that organizations can adapt to their specific needs.
Cultural changes such as wearing face masks are imperative for preventing the next pandemic from simultaneously crippling our health and economy. These cultural changes don’t just need to feel good, they need to be based on hard data. Simulations help support these changes, but real data from actual epidemics is also needed to improve our responses. This chapter lists some effective strategies that take a unique approach to combating illness—and covering your mouth when you cough is also never a bad idea.